Healthcare
Cancer Prevention in the 21st Century: The Role of Diet and Lifestyle
Cancer remains one of the most formidable challenges in global health, claiming millions of lives every year despite advances in medical research and technology. The 21st century has seen significant strides in the understanding and treatment of cancer. Yet, prevention remains a cornerstone of public health strategies aimed at reducing the incidence of this devastating disease. Among the various factors contributing to cancer prevention, diet and lifestyle play crucial roles. This article explores the intricate relationship between these factors and cancer prevention, shedding light on how modern lifestyle choices can either mitigate or exacerbate the risk of developing cancer.
The Epidemiology of Cancer: A Global Perspective
Cancer is not a single disease but a group of related diseases characterized by the uncontrolled division of abnormal cells. It can occur in almost any part of the body, leading to over 100 different types of cancer. According to the World Health Organization (WHO), cancer is the second leading cause of death globally, responsible for an estimated 9.6 million deaths in 2018 alone. Lung, breast, colorectal, prostate, and stomach cancers are among the most common types, contributing to a significant proportion of the global cancer burden.
The incidence of cancer varies significantly across different regions, reflecting variations in genetic predisposition, environmental exposures, lifestyle factors, and healthcare infrastructure. In high-income countries, lifestyle-related cancers, such as lung, breast, and colorectal cancer, are more prevalent. In contrast, in low- and middle-income countries, infections-related cancers, such as cervical and liver cancer, are more common.
The Role of Diet in Cancer Prevention
Diet is a modifiable risk factor with a profound impact on cancer development. A healthy diet can help prevent cancer by providing essential nutrients that support immune function, reduce inflammation, and neutralize harmful free radicals. Conversely, poor dietary habits can increase the risk of cancer by promoting obesity, chronic inflammation, and oxidative stress. The following sections explore how specific dietary components influence cancer risk.
-
Fruits and Vegetables: Nature’s Protective Shield
Fruits and vegetables are rich in vitamins, minerals, fiber, and phytochemicals, which have been shown to reduce the risk of various cancers. Phytochemicals, such as flavonoids, carotenoids, and polyphenols, possess antioxidant properties that protect cells from DNA damage caused by free radicals. Additionally, some phytochemicals can modulate carcinogen metabolism, enhance immune function, and inhibit tumor growth.
Numerous epidemiological studies have demonstrated an inverse relationship between fruit and vegetable consumption and the risk of cancers such as lung, colorectal, stomach, and esophageal cancer. For instance, a study published in the “Journal of the National Cancer Institute” found that a high intake of cruciferous vegetables, such as broccoli and cauliflower, was associated with a lower risk of lung cancer, particularly among smokers.
-
Fiber: A Key Player in Colorectal Cancer Prevention
Dietary fiber in whole grains, fruits, vegetables, and legumes plays a significant role in colorectal cancer prevention. Fiber promotes regular bowel movements, which helps to remove carcinogenic substances from the colon. Additionally, the fermentation of fiber by gut bacteria produces short-chain fatty acids, such as butyrate, which have anti-inflammatory and anti-carcinogenic properties.
A large-scale study published in “The Lancet” confirmed that high fiber intake is associated with a reduced risk of colorectal cancer. The study found that for every 10 grams of daily fiber intake, the risk of colorectal cancer decreased by 10%. This protective effect is particularly strong for fiber from cereal sources.
-
Red and Processed Meats: A Double-Edged Sword
While meat is a valuable source of protein and essential nutrients, excessive consumption of red and processed meats has been linked to an increased risk of several cancers, particularly colorectal cancer. The International Agency for Research on Cancer (IARC), a part of WHO, has classified processed meat as a Group 1 carcinogen, meaning there is sufficient evidence that it causes cancer in humans. Red meat, on the other hand, is classified as a Group 2A carcinogen, indicating that it is probably carcinogenic to humans.
The carcinogenic potential of red and processed meats is attributed to several factors. These include the presence of heme iron, which can promote the formation of N-nitroso compounds, known carcinogens. Additionally, cooking methods such as grilling or frying at high temperatures can lead to the formation of heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs), both of which have been shown to increase cancer risk.
-
Dietary Fats: Balancing the Good and the Bad
The type and amount of dietary fat consumed can influence cancer risk. While high intake of saturated fats and trans fats has been associated with an increased risk of certain cancers, such as breast and colorectal cancer, other fats may have protective effects. For example, omega-3 fatty acids in fatty fish like salmon and flaxseeds have anti-inflammatory properties that may help reduce cancer risk.
A study published in the “Journal of the American Medical Association” found that women with a higher intake of omega-3 fatty acids had a lower risk of breast cancer. The researchers suggested that omega-3 fatty acids might inhibit tumor growth by suppressing the production of pro-inflammatory cytokines and modulating the expression of genes involved in cancer progression.
-
Sugars and Refined Carbohydrates: The Role in Obesity-Related Cancers
High consumption of sugars and refined carbohydrates, such as white bread and sugary beverages, can contribute to obesity, which is a well-established risk factor for several cancers, including breast, colorectal, endometrial, and pancreatic cancer. Obesity promotes cancer development through various mechanisms, including chronic inflammation, insulin resistance, and altered levels of sex hormones.
Reducing the intake of added sugars and opting for whole grains and low-glycemic index foods can help maintain a healthy weight and reduce cancer risk. The American Institute for Cancer Research (AICR) recommends limiting the consumption of sugary drinks and energy-dense foods as part of a cancer-preventive diet.
The Role of Lifestyle in Cancer Prevention
In addition to diet, several lifestyle factors influence cancer risk. These include physical activity, tobacco use, alcohol consumption, and exposure to environmental carcinogens. The following sections discuss the impact of these factors on cancer prevention.

-
Physical Activity: Moving Towards a Healthier Future
Regular physical activity is a powerful tool for cancer prevention. It helps maintain a healthy weight, reduces inflammation, and improves immune function, which can lower cancer risk. Physical activity has been shown to reduce the risk of several cancers, including breast, colorectal, endometrial, and prostate cancer.
A study published in the “British Journal of Sports Medicine” found that individuals who engaged in the highest levels of physical activity had a 20% lower risk of developing cancer compared to those who were least active. The protective effect of physical activity is particularly strong for colorectal cancer, with studies showing that regular exercise can reduce the risk by up to 50%.
The American Cancer Society (ACS) recommends that adults engage in at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity physical activity per week. This can include activities such as brisk walking, cycling, swimming, or running.
-
Tobacco Use: The Leading Preventable Cause of Cancer
Tobacco use is the single most significant preventable cause of cancer. It is responsible for approximately 22% of cancer deaths worldwide and is strongly associated with lung, mouth, throat, esophageal, and pancreatic cancers, among others. Cigarette smoke contains over 70 known carcinogens, including polycyclic aromatic hydrocarbons, nitrosamines, and formaldehyde, which can damage DNA and promote cancer development.
Quitting smoking is the most effective way to reduce cancer risk. Studies have shown that the risk of lung cancer decreases significantly within 10 years of quitting, and the risk of other smoking-related cancers also declines over time. Public health campaigns, smoking cessation programs, and policies that restrict tobacco advertising and sales have played a crucial role in reducing tobacco use and associated cancer risk.
-
Alcohol Consumption: A Risk Factor in Moderation
Alcohol consumption is another modifiable risk factor for cancer. It has been linked to an increased risk of cancers of the mouth, throat, esophagus, liver, breast, and colon. The risk of cancer increases with the amount of alcohol consumed, with heavy drinkers facing the highest risk.
The mechanisms by which alcohol increases cancer risk include the conversion of ethanol to acetaldehyde, a toxic metabolite that can damage DNA and proteins. Alcohol can also increase the levels of estrogen, a hormone associated with breast cancer, and facilitate the absorption of other carcinogens, such as those found in tobacco smoke.
To reduce cancer risk, the AICR recommends limiting alcohol consumption to no more than two drinks per day for men and one drink per day for women. For individuals at high risk of alcohol-related cancers, complete abstinence may be the best strategy.
-
Environmental Carcinogens: Minimizing Exposure
Exposure to environmental carcinogens, such as asbestos, radon, air pollution, and certain chemicals, can increase cancer risk. Occupational exposure to carcinogens, such as benzene, formaldehyde, and vinyl chloride, is a significant concern in certain industries, including construction, manufacturing, and chemical production.
Minimizing exposure to environmental carcinogens is essential for cancer prevention. This can be achieved through workplace safety regulations, the use of protective equipment, and reducing exposure to air pollution. Additionally, individuals can reduce their risk by avoiding the use of certain chemicals in household products and by testing their homes for radon, a radioactive gas that is a leading cause of lung cancer.
The Role of Public Health and Policy in Cancer Prevention
While individual choices regarding diet and lifestyle are critical for cancer prevention, public health initiatives and policies also play a vital role. Governments, healthcare organizations, and community groups can implement strategies to promote healthy behaviors, reduce exposure to carcinogens, and increase access to preventive healthcare services. The following sections highlight key public health and policy approaches to cancer prevention.
-
Promoting Healthy Eating and Physical Activity
Public health campaigns that promote healthy eating and physical activity are essential for cancer prevention. These campaigns can raise awareness of the link between diet, lifestyle, and cancer risk, and provide practical tips for making healthier choices. For example, initiatives like “5 A Day” encourage people to eat at least five servings of fruits and vegetables daily, while programs like “Move Your Way” promote regular physical activity.
Schools, workplaces, and communities can also play a role by creating environments that support healthy behaviors. This can include providing access to healthy foods in cafeterias, promoting physical activity through exercise programs or walking paths, and offering incentives for participation in wellness programs.
-
Tobacco Control Policies
Tobacco control policies are among the most effective public health strategies for cancer prevention. These policies include measures such as increasing tobacco taxes, implementing smoke-free laws, restricting tobacco advertising, and providing access to smoking cessation services. Countries that have implemented comprehensive tobacco control policies have seen significant declines in smoking rates and tobacco-related cancers.
In addition to traditional tobacco products, there is growing concern about the use of electronic cigarettes (e-cigarettes) and other vaping devices. While e-cigarettes may be less harmful than traditional cigarettes, they are not without risk, and their long-term effects on cancer risk are not yet fully understood. Public health policies should address the use of these products, particularly among youth, to prevent a new generation from becoming addicted to nicotine.
-
Alcohol Control Policies
Alcohol control policies can also contribute to cancer prevention by reducing alcohol consumption at the population level. These policies may include increasing alcohol taxes, restricting the availability of alcohol, regulating alcohol advertising, and implementing public awareness campaigns about the link between alcohol and cancer.
For example, some countries have introduced minimum unit pricing for alcohol, which sets a floor price for alcoholic beverages to reduce excessive drinking. Such measures have been shown to be effective in reducing alcohol-related harm, including the risk of alcohol-related cancers.
-
Screening and Early Detection
Screening and early detection are critical components of cancer prevention. Early detection of cancer through screening can lead to more effective treatment and improved survival rates. For example, screening for cervical cancer using Pap smears and HPV testing has led to significant reductions in cervical cancer incidence and mortality.
Public health programs that promote and provide access to cancer screening can help detect cancer at an early, more treatable stage. These programs often target high-risk populations and provide education about the importance of regular screening. For example, mammography screening programs for breast cancer and colonoscopy screening programs for colorectal cancer have been instrumental in reducing mortality from these cancers.
-
Vaccination Programs
Vaccination against cancer-causing infections is another crucial public health strategy for cancer prevention. The introduction of the human papillomavirus (HPV) vaccine has been a major milestone in preventing cervical cancer, as well as other cancers caused by HPV, such as anal, oropharyngeal, and penile cancers. Similarly, vaccination against hepatitis B virus (HBV) has been shown to reduce the risk of liver cancer.
Public health initiatives that promote vaccination, particularly among adolescents and high-risk populations, can significantly reduce the burden of infection-related cancers. Ensuring access to vaccines in low- and middle-income countries, where the incidence of these cancers is often higher, is a global health priority.
The Future of Cancer Prevention: Emerging Trends and Challenges
As we move further into the 21st century, the landscape of cancer prevention is evolving, with new challenges and opportunities on the horizon. Advances in genomics, precision medicine, and technology are opening new avenues for personalized cancer prevention strategies. However, these advances also come with challenges, including disparities in access to preventive care, the impact of environmental changes, and the rise of new risk factors.
-
Personalized Nutrition and Cancer Prevention
The field of nutrigenomics, which studies the interaction between genetics and nutrition, holds promise for personalized cancer prevention. Understanding an individual’s genetic makeup can provide insights into how their body responds to different foods and nutrients, allowing for tailored dietary recommendations that optimize cancer prevention.
For example, individuals with certain genetic variants may be more susceptible to the carcinogenic effects of red meat or may benefit more from a diet rich in specific phytochemicals. As research in this area progresses, personalized nutrition could become a key component of cancer prevention strategies.
-
The Impact of Climate Change on Cancer Risk
Climate change poses new challenges for cancer prevention. Rising temperatures and changes in weather patterns can influence the prevalence of certain cancers by altering exposure to environmental carcinogens, such as air pollution and ultraviolet (UV) radiation. Additionally, climate change can impact food security and nutrition, potentially increasing the risk of diet-related cancers.
Addressing the links between climate change and cancer requires a multidisciplinary approach that considers environmental, social, and economic factors. Public health strategies must adapt to these changing conditions to effectively mitigate cancer risk in a warming world.
-
The Rise of Digital Health and Telemedicine
The rise of digital health technologies, including telemedicine, mobile health apps, and wearable devices, offers new opportunities for cancer prevention. These technologies can facilitate the monitoring of dietary and lifestyle behaviors, provide personalized feedback, and support adherence to preventive measures.
For example, mobile apps that track physical activity and diet can help individuals make healthier choices, while telemedicine platforms can increase access to cancer screening and preventive care, particularly in underserved areas. However, the integration of these technologies into public health initiatives requires careful consideration of privacy, data security, and equity issues.
-
Addressing Disparities in Cancer Prevention
Despite advances in cancer prevention, disparities in cancer incidence and outcomes persist, particularly among low-income and minority populations. These disparities are often driven by differences in access to healthcare, education, healthy foods, and safe environments.
Addressing these disparities requires targeted public health interventions that prioritize equity and inclusion. This includes expanding access to preventive services, such as cancer screening and vaccination, in underserved communities, as well as addressing social determinants of health, such as poverty and education, that contribute to cancer risk.
Conclusion
Cancer prevention in the 21st century is a multifaceted challenge that requires a comprehensive approach, integrating diet, lifestyle, public health policies, and emerging technologies. While significant progress has been made, there is still much work to be done to reduce the global burden of cancer. By making informed choices about diet and lifestyle, individuals can significantly reduce their risk of developing cancer. At the same time, public health initiatives and policies must continue to promote healthy behaviors, reduce exposure to carcinogens, and ensure equitable access to preventive care. As we look to the future, continued research and innovation will be essential in developing personalized cancer prevention strategies that can adapt to the evolving landscape of cancer risk.
-
 Press Release5 days ago
Press Release5 days agoCrypto WINNAZ Launches First On-Chain Yield Engine for Meme Coins, Enabling 20x–300x Returns
-

 Press Release3 days ago
Press Release3 days agoBellarium ($BEL) Price Prediction: Could It Hit $5 by 2026?
-
 Press Release23 hours ago
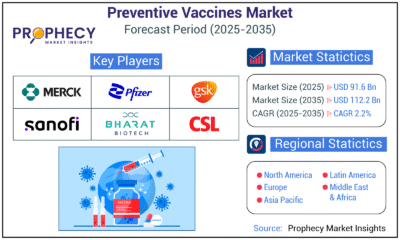
Press Release23 hours agoPreventive Vaccines Market to Witness Strong Growth by 2035
-

 Press Release3 days ago
Press Release3 days agoWhy Alaxio (ALX) Is a Top Pick for Smart Crypto Investors
-

 Business2 days ago
Business2 days agoHow Managed IT Solutions Help Small Teams Compete at Enterprise Scale
-
 Press Release23 hours ago
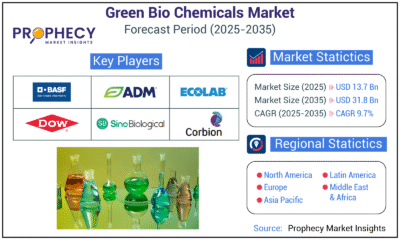
Press Release23 hours agoGreen Bio Chemicals Market Poised for Sustainable Growth amidst Global Shift to Eco-Friendly Alternatives by 2035
-
 Press Release23 hours ago
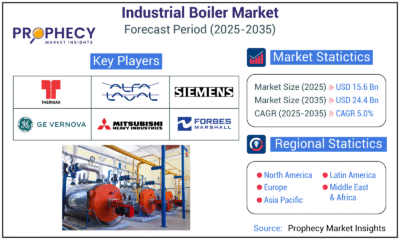
Press Release23 hours agoIndustrial Boiler Market Expected to Surpass USD 24.4 Billion by 2035 Amid Growing Demand for Energy Efficiency and Industrialization
-

 Press Release23 hours ago
Press Release23 hours agoCat Food Market Forecast 2035: Natural Ingredients, Pet Wellness to Lead the Way