Canada News
The Economic Consequences of Nurse Burnout and Turnover in Healthcare Systems

Image Source: vecteezy.com
The health industry is fast-paced and very demanding, and nurses play a pivotal role in keeping the industry moving. However, the relentless pressures they face can lead to burnout which is a pervasive issue with significant economic consequences for healthcare systems.
Nurse burnout, characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment, impacts the well-being of healthcare professionals and affects the financial stability and quality of care within healthcare organizations. This article will talk about nurse burnout, turnover, and their economic and other implications for the industry.
Understanding Nurse Burnout and Turnover
Nurse burnout is a result of chronic workplace stress that has not been successfully managed. It is often characterized by feelings of emotional exhaustion, depersonalization, and reduced personal accomplishment.
Factors contributing to nurse burnout include long working hours, high patient loads, administrative burdens, inadequate staffing, and exposure to emotionally charged situations. These factors, compounded with frequent overtime, can lead to a decline in job satisfaction, mental health issues, and ultimately, an increased likelihood of nurses leaving their positions.
Nurse turnover, on the other hand, refers to the rate at which nurses leave their jobs within a specified period. High turnover rates in healthcare settings are often linked to burnout and can have detrimental effects on organizational stability and patient care.
When experienced and skilled nurses leave, it disrupts continuity of care, increases workload for remaining staff, and necessitates costly recruitment and training processes.
Understanding the relationship between burnout and turnover is crucial so that healthcare organizations can develop targeted strategies that will improve nurse well-being, enhance job satisfaction, and ultimately, mitigate the economic impact of these issues.
Economic Costs of Nurse Burnout
The economic costs associated with nurse burnout affect both the specific healthcare organization and the broader healthcare industry. Various research and studies have highlighted the significant financial burden that nurse burnout places on healthcare systems. For example, a 2018 study estimated that nurse turnover costs healthcare organizations between $4.4 million and $7 million annually per hospital.
These costs cover recruitment, training, lost productivity, and other expenses associated with turnover-induced disruptions in care delivery.
Economic costs can be further categorized into direct and indirect expenses, all of which contribute to financial strain and operational challenges within healthcare settings.
Direct Costs
Direct costs include expenses directly related to managing and mitigating nurse burnout. These may include recruitment and hiring costs to replace nurses who leave due to burnout, expenses for training new staff members, overtime pay to cover staffing shortages, and the use of temporary staffing agencies to fill gaps in the workforce.
Additionally, healthcare organizations may incur costs for employee assistance programs, counseling services, and other interventions aimed at addressing burnout among nursing staff.
Indirect Costs
Indirect costs include the broader impact of nurse burnout on organizational productivity, quality of care, and patient outcomes.
Burnout can cause decreased productivity among nurses, resulting in lower efficiency and effectiveness in delivering care, which contributes to increased patient wait times, delays in treatment, and overall dissatisfaction among patients.
Moreover, burnout is associated with higher rates of medical errors and adverse events, which can lead to costly litigation, penalties, and damage to the organization’s reputation.
Strategies to Address Nurse Burnout and Turnover
- Employee Support Programs
Healthcare organizations should offer comprehensive employee support programs that provide access to mental health services, counseling, and stress management resources. These programs empower nurses to seek help when needed and prioritize their well-being.
- Workload Management
Implementing workload management strategies such as appropriate staffing levels, workload distribution, and scheduling practices can help prevent burnout by reducing excessive workloads and ensuring adequate rest and recovery time for nurses.
- Training and Education
Providing training and education on stress management techniques, resilience-building skills, and self-care practices equips nurses with the tools they need to cope with the demands of their jobs effectively. This can include workshops, seminars, and online resources tailored to the needs of nursing staff.
- Leadership Support
Strong leadership support is crucial in creating a positive work culture that values and prioritizes employee well-being.
Engaging leaders who actively listen to staff concerns, advocate for work-life balance, and promote open communication can foster a supportive and inclusive work environment.
- Recognition and Rewards
Recognizing and rewarding nurses for their hard work, dedication, and contributions can boost morale, motivation, and job satisfaction. This can include incentive programs, recognition ceremonies, and opportunities for professional growth and development.
- Work-Life Balance Initiatives
It’s important to offer work-life balance initiatives like flexible scheduling options, remote work opportunities (where feasible), and paid time off policies to nurses.
These support work-life balance and can help prevent burnout and improve retention rates among nursing staff.
How Home Health and/or (Certified) Nursing Assistants Can Help in Alleviating Nurse Burnout
- Reduced Workload
Home health aides,(Certified) Nursing Assistants, and/or SNFists help lighten the workload for nurses by taking on some of the tasks that nurses would otherwise have to perform themselves.
Reduction in workloads allows nurses to focus more on clinical care and complex medical tasks, reducing the stress and physical demands of their jobs.
- Improved Work-Life Balance
Nurses often struggle with maintaining a healthy work-life balance due to long hours and demanding schedules. Home health services enable patients to receive care in the comfort of their homes, reducing the need for extended hospital stays or frequent clinic visits. This flexibility allows nurses to have more predictable schedules and time for self-care, family, and personal activities, reducing burnout risk.
- Comprehensive Care Coordination
Home healthcare facilitates seamless care coordination between healthcare professionals, patients, and families.
Health aides work collaboratively with nurses, therapists, and other team members to ensure continuity of care, adherence to treatment plans, and effective communication, reducing the administrative burden on nurses and promoting efficient care delivery.
Conclusion
Nurse burnout and turnover pose significant economic challenges for healthcare systems, affecting organizational stability, patient care quality, and overall financial health.
Healthcare organizations can mitigate the economic costs of nurse burnout and turnover by implementing employee support programs, fostering strong leadership support, and promoting work-life balance initiatives, among others.
In addition, home healthcare services can help healthcare systems navigate the economic challenges posed by nurse burnout and turnover more effectively, ultimately benefiting both healthcare professionals and the patients they serve.
-

 Press Release6 days ago
Press Release6 days agoNura Labs Files Revolutionary Patent: AI-Powered Wallet Solves the $180 Billion Crypto Staking Complexity Crisis
-
 Press Release4 days ago
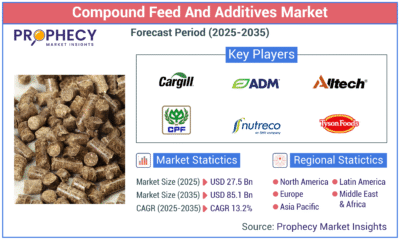
Press Release4 days agoGlobal Compound Feeds and Additives Industry Report: Market Expansion and Competitive Insights to 2035
-

 Technology4 days ago
Technology4 days agoWhat to Know Before Switching Cell Phone Network Services in 2025
-
 Press Release2 days ago
Press Release2 days agoCrypto WINNAZ Launches First On-Chain Yield Engine for Meme Coins, Enabling 20x–300x Returns


































