Public Health
Hepatitis (A, B, C): Understanding the Differences and Preventing Infection
Hepatitis is a term that refers to inflammation of the liver, often caused by a viral infection. According to the World Health Organization (WHO), viral hepatitis remains a major public health concern, affecting millions of people worldwide and resulting in significant morbidity and mortality. This report provides an in-depth understanding of Hepatitis A, B, and C, highlighting their differences, transmission routes, symptoms, and prevention strategies.
Hepatitis A: Overview, Transmission, and Prevention
Hepatitis A (HAV) is a highly contagious liver infection caused by the Hepatitis A virus. Unlike Hepatitis B and C, it does not lead to chronic liver disease but can cause debilitating symptoms and acute liver failure in rare cases. The WHO estimates that there are approximately 1.5 million cases of Hepatitis A each year globally.
- Transmission: Hepatitis A is primarily transmitted through the ingestion of contaminated food and water or close contact with an infected person. Poor sanitation and inadequate access to clean water significantly increase the risk of HAV outbreaks, especially in developing countries. The Centers for Disease Control and Prevention (CDC) also notes that travelers to regions with high HAV prevalence, such as parts of Africa, Asia, and Central and South America, are at increased risk.
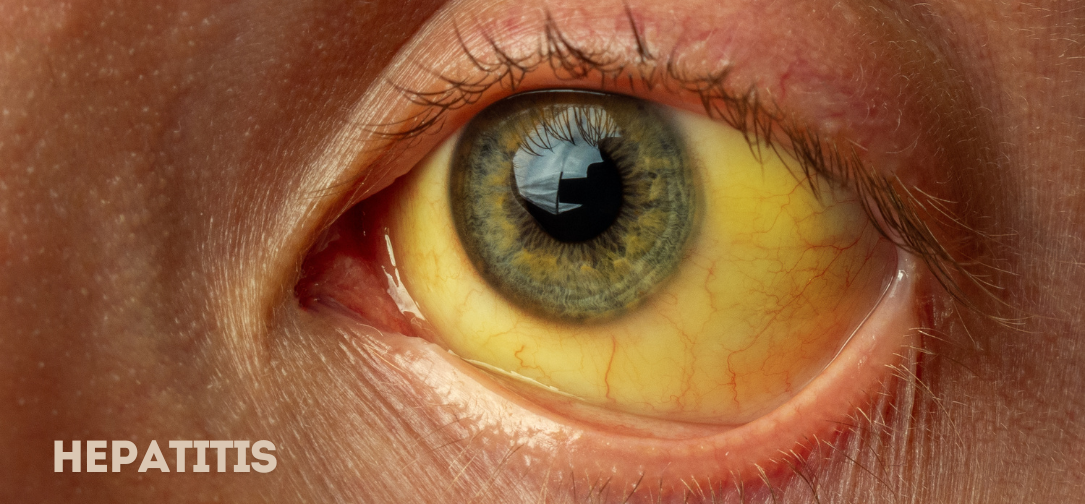
- Symptoms: Symptoms of Hepatitis A include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, jaundice (yellowing of the skin and eyes), dark urine, and pale stool. These symptoms typically appear two to six weeks after exposure and can last for several weeks to months. While most people recover fully without long-term effects, some may experience prolonged illness.
- Prevention: The most effective way to prevent Hepatitis A is through vaccination. The CDC recommends Hepatitis A vaccination for all children at the age of one year, travelers to countries with high HAV rates, men who have sex with men, and individuals with chronic liver diseases. Good hygiene practices, such as regular hand washing and safe food and water consumption, are also essential preventive measures.
- Current Statistics: In recent years, there have been sporadic outbreaks of Hepatitis A in various parts of the world, including the United States and Europe, often linked to contaminated food or water sources. The CDC reported a significant increase in Hepatitis A cases in the U.S. between 2016 and 2020, with over 33,000 reported cases and 61 deaths, primarily among unvaccinated adults.
Hepatitis B: Overview, Transmission, and Prevention
Hepatitis B (HBV) is a serious liver infection caused by the Hepatitis B virus. Unlike Hepatitis A, Hepatitis B can cause both acute and chronic infections. According to the WHO, an estimated 296 million people worldwide were living with chronic Hepatitis B infection in 2019, with about 1.5 million new infections each year.
- Transmission: Hepatitis B is transmitted through contact with infectious body fluids, such as blood, semen, and vaginal secretions. Common modes of transmission include perinatal transmission from mother to child during childbirth, unsafe injection practices, transfusions of unscreened blood, sexual contact with an infected person, and sharing needles among drug users. The WHO emphasizes that healthcare settings with poor infection control practices pose significant risks for HBV transmission.
- Symptoms: Acute Hepatitis B infection may present with symptoms such as jaundice, dark urine, extreme fatigue, nausea, vomiting, and abdominal pain. While some individuals, especially young children, may remain asymptomatic, others develop severe illness. Chronic Hepatitis B can lead to long-term health issues, including cirrhosis, liver failure, and hepatocellular carcinoma (liver cancer).
- Prevention: The Hepatitis B vaccine is the most effective way to prevent infection. The WHO recommends that all infants receive the Hepatitis B vaccine as soon as possible after birth, preferably within 24 hours. For adults, the vaccine is recommended for those at high risk, including healthcare workers, people who inject drugs, and individuals with multiple sexual partners. The CDC also advises screening for HBV in pregnant women to prevent perinatal transmission.
- Current Statistics: The global burden of Hepatitis B remains substantial, particularly in low- and middle-income countries. In 2019, the WHO reported that approximately 820,000 people died from Hepatitis B, primarily due to cirrhosis and liver cancer. The WHO has set a target to eliminate viral hepatitis as a public health threat by 2030, aiming for a 90% reduction in new cases and a 65% reduction in mortality.
Hepatitis C: Overview, Transmission, and Prevention
Hepatitis C (HCV) is a liver infection caused by the Hepatitis C virus. It is often referred to as a “silent” epidemic because most people with HCV do not have symptoms until the infection has progressed to more severe liver damage. The WHO estimates that 58 million people globally have chronic Hepatitis C, with approximately 1.5 million new infections each year.
- Transmission: Hepatitis C is primarily spread through blood-to-blood contact. The most common routes of transmission include sharing needles and syringes among people who inject drugs, unscreened blood transfusions and organ transplants, and inadequate sterilization of medical equipment. Unlike Hepatitis B, sexual transmission of HCV is less common but can occur, particularly among people with multiple sexual partners or coexisting sexually transmitted infections.
- Symptoms: Acute Hepatitis C infection is often asymptomatic or may present with mild symptoms, such as fever, fatigue, jaundice, dark urine, and joint pain. Chronic Hepatitis C, if left untreated, can lead to severe complications such as cirrhosis, liver cancer, and liver failure over several decades.
- Prevention: Unlike Hepatitis A and B, there is currently no vaccine for Hepatitis C. Prevention strategies focus on reducing the risk of exposure to the virus. The CDC recommends harm reduction services for people who inject drugs, such as needle exchange programs and safe injection practices. Blood safety measures, including screening donated blood and organs, are also critical. The WHO advocates for targeted interventions, particularly in high-risk populations, to prevent new infections.
- Current Statistics: The global response to Hepatitis C has seen significant progress in recent years, particularly with the advent of highly effective direct-acting antiviral (DAA) treatments that can cure over 95% of cases. However, access to these treatments remains uneven, especially in low- and middle-income countries. The WHO has set ambitious goals to reduce new Hepatitis C infections by 80% and mortality by 65% by 2030.
Key Differences Between Hepatitis A, B, and C
While all three types of Hepatitis viruses affect the liver, they differ in terms of transmission, clinical course, and prevention strategies:
1. Transmission Routes:
- Hepatitis A: Primarily transmitted through fecal-oral routes, contaminated food, and water.
- Hepatitis B: Spread through contact with infected body fluids (blood, semen, vaginal fluids).
- Hepatitis C: Primarily spread through blood-to-blood contact.
2. Chronicity:
- Hepatitis A: Does not cause chronic infection.
- Hepatitis B: Can cause chronic infection, particularly in those infected at a young age.
- Hepatitis C: Often leads to chronic infection and is a major cause of liver-related complications.
3. Prevention Strategies:
- Hepatitis A: Vaccination, safe food and water practices, and good hygiene.
- Hepatitis B: Vaccination, safe sex practices, blood safety, and infection control in healthcare settings.
- Hepatitis C: No vaccine available; prevention focuses on harm reduction and blood safety.
Global Health Impact and Policy Recommendations
Viral hepatitis poses a significant global health challenge, particularly in regions with limited healthcare resources and access to vaccinations and treatments. The WHO’s Global Hepatitis Strategy (2016-2021) aimed to eliminate Hepatitis B and C as major public health threats by 2030, focusing on expanding vaccination coverage, enhancing blood and injection safety, improving infection control in healthcare settings, and increasing access to diagnosis and treatment.
Despite progress in some areas, challenges remain in achieving these goals. According to a recent report by the WHO, only 10% of people living with chronic Hepatitis B and 21% of those with Hepatitis C were aware of their infection status in 2021. Moreover, global disparities in access to life-saving treatments, such as DAAs for Hepatitis C, continue to hinder efforts to reduce hepatitis-related mortality.
Conclusion
Understanding the differences between Hepatitis A, B, and C is crucial for effective prevention, diagnosis, and treatment strategies. While significant strides have been made in combating these infections, achieving the goal of eliminating viral hepatitis as a public health threat by 2030 will require sustained global commitment, increased awareness, and equitable access to prevention and treatment services. As healthcare systems worldwide continue to grapple with the ongoing challenges of hepatitis, public health policies must prioritize comprehensive strategies to reduce the burden of these preventable infections. By focusing on education, vaccination, and harm reduction strategies, we can make substantial progress in reducing the global burden of Hepatitis A, B, and C and move closer to the goal of elimination by 2030.
-

 Business5 days ago
Business5 days agoS&P 500 Soars in Best May in Decades Amid Tariff Relief and Nvidia’s Surge
-

 Healthcare6 days ago
Healthcare6 days agoAttention Economy Arms Race: Reclaim Your Focus in a World Designed to Distract You
-

 Immigration5 days ago
Immigration5 days agoTrump’s Immigration Crackdown: Legal Battles and Policy Shifts
-

 Government5 days ago
Government5 days agoTrump Administration’s Government Reshaping Efforts Face Criticism and Legal Battles
-

 Business5 days ago
Business5 days agoUS Stock Market Soars in May Amidst Tariff Tensions and Inflation Worries
-

 Business5 days ago
Business5 days agoTrump’s Tariffs: A Global Economic Reckoning
-
 Foreign Policy2 days ago
Foreign Policy2 days agoInside Schedule F: Will Trump’s Federal Workforce Shake-Up Undermine Democracy?
-

 Press Release2 days ago
Press Release2 days agoIn2space Launches Campaign to Make Space Travel Accessible for All