Public Health
Sexually Transmitted Infections (STIs): Prevention, Treatment, and Myths

Sexually transmitted infections (STIs), often referred to as sexually transmitted diseases (STDs), remain a significant public health concern worldwide. Affecting millions of people annually, these infections can lead to severe health complications if not treated promptly. However, despite widespread awareness efforts, numerous myths and misconceptions about STIs persist, often hindering effective prevention and treatment strategies.
The Global Landscape of STIs
The prevalence of STIs varies by region, but certain infections are more common globally than others. Human papillomavirus (HPV) is the most prevalent STI in the United States, followed closely by herpes. Globally, chlamydia, gonorrhea, syphilis, and trichomoniasis also rank highly among the most common infections. According to the World Health Organization (WHO), more than one million STIs are acquired every day worldwide, with young people aged 15-24 being the most affected demographic.
Prevention Strategies
Preventing STIs involves a multi-faceted approach, including education, vaccination, and regular testing. One of the most effective methods of prevention is the consistent use of condoms, which significantly reduces the risk of contracting or spreading STIs during vaginal, anal, or oral sex. Vaccinations are also crucial, particularly for HPV and hepatitis B, which are both preventable through immunization.
Behavioral interventions, such as promoting abstinence, monogamy, or reducing the number of sexual partners, can also reduce STI risk. Public health campaigns often emphasize the importance of getting tested regularly, especially for sexually active individuals, as many STIs can be asymptomatic. Early detection through screening can prevent long-term health complications and reduce the spread of infections.
Treatment Options
The treatment of STIs varies depending on the type of infection. Bacterial infections such as chlamydia, gonorrhea, and syphilis can be effectively treated with antibiotics. However, early treatment is essential, as delayed intervention can lead to severe complications, including infertility and chronic pain.
For viral infections like herpes and HIV, while there is no cure, antiviral medications can manage symptoms, reduce the frequency of outbreaks, and lower the risk of transmission. For instance, antiretroviral therapy (ART) for HIV has transformed it from a fatal disease into a manageable chronic condition, significantly extending life expectancy and reducing transmission rates.
Additionally, for those exposed to HIV, pre-exposure prophylaxis (PrEP) is available as a preventive treatment, further reducing the risk of contracting the virus. Vaccines are also available for hepatitis B and HPV, offering protection against these viruses.
Addressing Common Myths and Misconceptions
Despite widespread information, several myths about STIs persist, often leading to stigma and preventing individuals from seeking appropriate care. Here are some common myths and the truths behind them:
- Myth: STIs are only contracted through penetrative sex.
Truth: STIs can be transmitted through various forms of sexual activity, including oral sex and even deep kissing in some cases. For example, herpes (HSV-1 and HSV-2) can spread through skin-to-skin contact and saliva.
- Myth: You can’t get an STI if you’re in a monogamous relationship.
Truth: While monogamy reduces the risk of contracting STIs, it doesn’t eliminate it. Many individuals may unknowingly carry an STI from previous relationships, emphasizing the importance of regular testing for both partners.
- Myth: STIs can be contracted from toilet seats.
Truth: The likelihood of contracting an STI from a toilet seat is extremely low, as most viruses and bacteria cannot survive long outside the human body.
- Myth: Once you have an STI, your sex life is over.
Truth: Many STIs are treatable, and even those that are not curable, like herpes or HIV, can be managed with proper medical care, allowing individuals to continue healthy sexual relationships.
- Myth: Only people with multiple sexual partners get STIs.
Truth: Anyone who is sexually active is at risk of contracting an STI, regardless of the number of partners. Safe sexual practices and regular testing are key to prevention.
The Importance of Education and Awareness
Education is paramount in the fight against STIs. Comprehensive sexual education that covers safe sex practices, the importance of regular testing, and the realities of living with STIs can help dispel myths and reduce stigma. Public health initiatives should also focus on making testing and treatment more accessible, particularly for high-risk populations.
Awareness campaigns need to be culturally sensitive and inclusive, addressing the diverse needs of different communities. This includes providing resources in multiple languages, offering services in underserved areas, and using media that resonate with various age groups.
Emerging Trends and Future Directions
The landscape of STI prevention and treatment is continuously evolving. Advances in medical research are leading to the development of new vaccines and medicines. For example, research is ongoing into vaccines for herpes and even HIV, which could revolutionize the management of these infections.
Moreover, the integration of digital health technologies, such as telemedicine and home testing kits, is making it easier for individuals to access care and maintain their sexual health. These innovations are particularly important in reaching populations who may be reluctant to visit clinics due to stigma or privacy concerns.
However, these advancements must be accompanied by continued efforts to combat misinformation and ensure that everyone, regardless of socioeconomic status, has access to the necessary resources to prevent and treat STIs.
Recent Advances in STI Vaccines: Herpes, HIV, and HPV Developments
The landscape of vaccine development for Sexually Transmitted Infections (STIs) has seen significant advancements, particularly for Herpes, HIV, and Human Papillomavirus (HPV) vaccines, with some promising updates emerging in recent years.
Herpes Vaccine Development:
A significant development in herpes vaccine research is Moderna’s mRNA-1608 candidate, which entered its Phase 1/2 clinical trials in late 2023. This vaccine aims to address Herpes Simplex Virus Type 2 (HSV-2), responsible for genital herpes. The trial involves 300 participants with a history of recurrent genital herpes. The study is designed to test the vaccine’s safety, immunogenicity, and potential clinical benefits. While there is no FDA-approved herpes vaccine yet, Moderna’s mRNA technology, which proved highly effective during the COVID-19 pandemic, shows promise in this field as well
HIV Vaccine Progress:
In the realm of HIV vaccine research, the pursuit of a reliable vaccine has been ongoing for decades due to the virus’s rapid mutation rate and ability to evade the immune system. Recent breakthroughs involve the use of mRNA technology similar to that used in COVID-19 vaccines. A Phase 1 trial of a new HIV vaccine candidate, developed with nanoparticle technology, showed promising results. This vaccine, known as eOD-GT8 60-mer, successfully elicited a robust immune response in nearly all the 36 volunteers involved in the trial. The focus is now on combining multiple immunogens targeting different sites on the HIV envelope protein to induce the broadly neutralizing antibodies necessary to protect against various HIV strains.
HPV Vaccines:
While existing HPV vaccines like Gardasil are highly effective in preventing strains of HPV that cause cervical and other cancers, researchers continue to explore new formulations and delivery methods to broaden protection. The development of next-generation vaccines could potentially provide coverage against additional strains and improve long-term immunity.
These developments highlight the ongoing efforts in STI vaccine research. As trials progress, especially with innovative mRNA technology, the medical community remains hopeful that effective vaccines for these challenging infections will soon become available. These advancements underscore the potential of mRNA platforms and provide a foundation for future STI vaccine developments.
Conclusion
Understanding STIs, prevention, and treatment is crucial for public health. While significant strides have been made in reducing the burden of these infections, much work remains. Dispelling myths, promoting education, and ensuring access to testing and treatment are essential steps in combating the global STI epidemic. As we move forward, continued innovation in medical research, combined with robust public health strategies, will be vital to managing and eventually eradicating these infections.
-
 Press Release4 days ago
Press Release4 days agoClinical Trials Market Set for Robust Growth, Driven by Drug Development Surge and Digital Innovation
-

 Press Release5 days ago
Press Release5 days agoFill-Finish Pharmaceutical Contract Manufacturing Market Expected to Flourish Amid Biopharmaceutical Boom and Global Outsourcing Trend by 2035
-

 Press Release7 days ago
Press Release7 days agoBellarium ($BEL) Price Prediction: Could It Hit $5 by 2026?
-

 Business6 days ago
Business6 days agoHow Managed IT Solutions Help Small Teams Compete at Enterprise Scale
-
 Press Release5 days ago
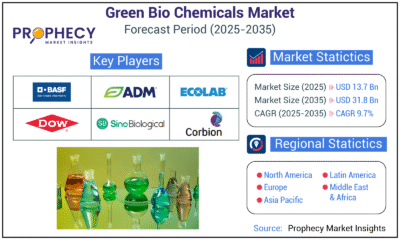
Press Release5 days agoGreen Bio Chemicals Market Poised for Sustainable Growth amidst Global Shift to Eco-Friendly Alternatives by 2035
-
 Press Release5 days ago
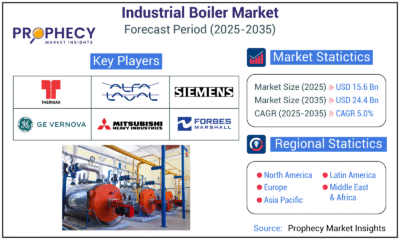
Press Release5 days agoIndustrial Boiler Market Expected to Surpass USD 24.4 Billion by 2035 Amid Growing Demand for Energy Efficiency and Industrialization
-
 Press Release5 days ago
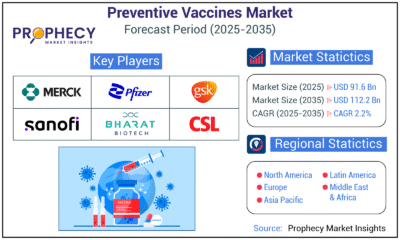
Press Release5 days agoPreventive Vaccines Market to Witness Strong Growth by 2035
-

 Press Release5 days ago
Press Release5 days agoPet Food Nutraceutical Market Set for Robust Expansion Amid Rising Demand for Pet Wellness by 2035