Healthcare
Overview of Current Industry Trends and Leading Changes in Public Health

Public health has always been at the forefront of addressing society’s most pressing health challenges. From controlling infectious diseases to promoting healthy lifestyles, public health professionals have played a crucial role in shaping the well-being of populations. However, the landscape of public health is constantly evolving, influenced by technological advancements, demographic shifts, environmental changes, and emerging global threats. This article provides a comprehensive overview of the current industry trends and leading changes in public health, highlighting the challenges, opportunities, and innovations shaping this vital field’s future.
The Evolving Landscape of Public Health
The field of public health is inherently dynamic, responding to the changing needs of populations and the emergence of new health threats. Several key trends have recently significantly impacted public health practices and policies. These trends include integrating digital health technologies, the rise of precision public health, the increasing focus on mental health, the challenges posed by climate change, and the growing emphasis on health equity and social determinants of health.
1) Digital Health and Technological Integration
One of the most transformative trends in public health today is the integration of digital health technologies. The advent of digital health tools, including mobile health (mHealth) applications, telemedicine, wearable devices, and artificial intelligence (AI), has revolutionized the delivery of public health services and the collection, analysis, and utilization of health data.
- Telemedicine and Remote Care: Telemedicine has become a cornerstone of modern healthcare, particularly during the COVID-19 pandemic, where it played a critical role in maintaining access to care while reducing the risk of virus transmission. Telemedicine platforms enable healthcare providers to deliver consultations, monitor patients, and provide follow-up care remotely. This has particularly benefited rural and underserved populations with limited access to healthcare facilities.
- Mobile Health Applications: mHealth applications have empowered individuals to take control of their health by providing tools for monitoring chronic conditions, managing medications, and tracking physical activity and nutrition. These apps have also been used in public health campaigns to promote healthy behaviors and disseminate important health information to the public.
- Wearable Devices and Health Monitoring: Wearable devices, such as fitness trackers and smartwatches, have gained popularity for their ability to monitor vital signs, track physical activity, and even detect early signs of disease. In public health, these devices offer the potential for real-time data collection, enabling more accurate and timely assessments of population health trends.
- Artificial Intelligence and Data Analytics: AI and data analytics are increasingly used in public health to analyze large datasets, predict disease outbreaks, and identify at-risk populations. AI-driven tools can process vast amounts of data from electronic health records (EHRs), social media, and other sources to provide insights that inform public health interventions and policies.
2) Precision Public Health
Precision public health is an emerging trend that aims to tailor public health interventions to specific populations or individuals based on their genetic, environmental, and lifestyle factors. This approach, which draws from the principles of precision medicine, seeks to improve the effectiveness of public health initiatives by targeting interventions more precisely.
- Genomic Epidemiology: Genomic epidemiology involves using genetic information to track the spread of infectious diseases and understand their origins. This approach has been instrumental in the response to the COVID-19 pandemic, where genomic sequencing was used to identify new variants of the virus and trace transmission patterns.
- Personalized Prevention: Precision public health also involves personalized prevention strategies, where interventions are tailored to an individual’s risk factors. For example, individuals with a genetic predisposition to certain diseases may receive targeted prevention measures, such as early screening and lifestyle modifications.
- Data-Driven Interventions: By leveraging big data and advanced analytics, precision public health can identify subpopulations at higher risk for certain health outcomes. This allows for the development of targeted interventions that are more likely to effectively reduce health disparities and improve overall population health.
3) Mental Health as a Public Health Priority
Mental health has traditionally been underrepresented in public health initiatives, but this is rapidly changing as the burden of mental health disorders becomes more apparent. The increasing recognition of mental health as a public health priority leads to new prevention, treatment, and policy approaches.
- Integration of Mental Health into Primary Care: One of the leading changes in public health is integrating mental health services into primary care. This approach aims to reduce the stigma associated with mental health disorders and improve access to care by making mental health services available within general healthcare settings.
- Community-Based Mental Health Programs: Community-based mental health programs are becoming increasingly popular to provide accessible and culturally appropriate care. These programs often involve partnerships between public health agencies, non-governmental organizations (NGOs), and community groups to deliver mental health services and support.
- Digital Mental Health Interventions: Digital health technologies are also being used to address mental health needs. Apps that provide cognitive-behavioral therapy (CBT), stress management tools, and peer support networks are becoming widely available, offering new ways for individuals to access mental health care.
- Policy and Advocacy: Public health professionals are increasingly involved in advocating for mental health policies that promote access to care, reduce stigma, and address the social determinants of mental health. This includes efforts to integrate mental health into public health strategies and ensure that mental health is considered in all policies.
4) Climate Change and Environmental Health
Climate change is one of the most significant global health threats of the 21st century, with far-reaching impacts on public health. The effects of climate change, such as extreme weather events, rising temperatures, and changing disease patterns, are challenging public health systems and requiring new approaches to environmental health.
- Climate Resilience and Adaptation: Public health agencies are increasingly focused on building climate resilience by developing strategies to adapt to the health impacts of climate change. This includes preparing for and responding to extreme weather events, such as hurricanes, floods, and heatwaves, which can devastate health.
- Vector-Borne Diseases: Climate change also influences the spread of vector-borne diseases, such as malaria, dengue, and Zika. As temperatures rise and weather patterns shift, the habitats of disease-carrying vectors like mosquitoes are expanding, leading to increased transmission in new areas. Public health efforts are focused on monitoring these changes and implementing vector control measures.
- Environmental Justice: The concept of environmental justice is gaining traction in public health, recognizing that marginalized communities are disproportionately affected by environmental hazards and climate change. Public health professionals are advocating for policies that address these disparities and ensure that all communities have access to clean air, water, and safe living conditions.
- Sustainable Public Health Practices: There is a growing emphasis on sustainability in public health practices, including efforts to reduce the carbon footprint of healthcare facilities, promote active transportation, and advocate for policies that support sustainable development.
5) Health Equity and Social Determinants of Health
Health equity, which aims to ensure that everyone has a fair and just opportunity to achieve optimal health, is a central focus of modern public health. Addressing the social determinants of health; such as income, education, housing, and access to healthcare is critical to achieving health equity.
- Social Determinants of Health: Public health initiatives are increasingly addressing the social determinants of health by targeting the root causes of health disparities. This includes efforts to improve access to education, create affordable housing, reduce food insecurity, and address systemic racism and discrimination.
- Community-Driven Approaches: Engaging communities in the design and implementation of public health programs is essential for addressing health inequities. Community-driven approaches ensure that interventions are culturally relevant, responsive to local needs, and sustainable.
- Health in All Policies (HiAP): The HiAP approach is gaining momentum as a way to promote health equity by integrating health considerations into all areas of policy-making, including transportation, housing, education, and employment. HiAP encourages cross-sector collaboration to address the social determinants of health and create environments that support health for all.
- Global Health Equity: Public health professionals are also focusing on global health equity, advocating for policies and programs that address health disparities between and within countries. This includes efforts to improve access to essential medicines, strengthen health systems in low- and middle-income countries, and promote global solidarity in health.
6) The Impact of Pandemics on Public Health
The COVID-19 pandemic has had a profound impact on public health, highlighting the need for stronger global health systems, better pandemic preparedness, and more resilient healthcare infrastructure. The lessons learned from the pandemic are driving changes in public health practices and policies.
- Pandemic Preparedness and Response: The COVID-19 pandemic exposed gaps in pandemic preparedness and response, leading to calls for reform at the national and global levels. Public health agencies are now focusing on strengthening surveillance systems, improving coordination and communication, and investing in research and development for vaccines and treatments.
- Health System Strengthening: The pandemic has underscored the importance of strong health systems that can withstand the pressures of a public health crisis. This includes building capacity in areas such as critical care, laboratory testing, and supply chain management, as well as ensuring that healthcare workers are adequately trained and protected.
- Vaccine Distribution and Equity: The global rollout of COVID-19 vaccines has highlighted challenges related to vaccine distribution and equity. Public health efforts are now focused on ensuring that vaccines are distributed fairly, both within and between countries, and that all populations have access to life-saving vaccines.
- Mental Health and Resilience: The mental health impact of the pandemic has been significant, with increased rates of anxiety, depression, and burnout among healthcare workers and the general population. Public health strategies are being developed to address these mental health challenges and build resilience in the face of future crises.
7) The Role of Policy and Governance in Public Health
Policy and governance play a critical role in shaping public health outcomes. Effective public health policies are essential for addressing health challenges, promoting healthy behaviors, and ensuring that health systems are responsive to the needs of the population.
- Health Policy and Legislation: Public health professionals are increasingly involved in the development and implementation of health policies and legislation. This includes advocating for policies that promote healthy environments, protect vulnerable populations, and address emerging health threats.
- Global Health Governance: The governance of global health is evolving in response to the challenges posed by pandemics, climate change, and other global health threats. International organizations, such as the World Health Organization (WHO), are playing a key role in coordinating global health efforts and ensuring that all countries have access to the resources they need to protect public health.
- Public Health Leadership: Effective leadership is essential for advancing public health goals and responding to health challenges. Public health leaders are responsible for setting the vision and direction for public health initiatives, building partnerships, and mobilizing resources to achieve public health objectives.
- Public Health Advocacy: Advocacy is a powerful tool for advancing public health policies and promoting health equity. Public health professionals are increasingly engaged in advocacy efforts, working to influence policy-makers, raise public awareness, and mobilize communities to take action on health issues.
8) Education and Workforce Development in Public Health
As public health continues to evolve, so too must the education and training of public health professionals. Ensuring that the public health workforce is equipped with the skills and knowledge needed to address current and future health challenges is a key priority.
- Interdisciplinary Education: Public health education is becoming increasingly interdisciplinary, reflecting the complex and interconnected nature of health challenges. This approach emphasizes the importance of collaboration across disciplines, such as epidemiology, biostatistics, environmental health, social sciences, and health policy.
- Workforce Development: Developing a strong public health workforce requires ongoing training and professional development opportunities. This includes providing access to continuing education, mentoring programs, and leadership development initiatives to ensure that public health professionals are prepared to take on leadership roles and respond to emerging health threats.
- Diversity and Inclusion in Public Health: Promoting diversity and inclusion within the public health workforce is essential for addressing health disparities and ensuring that public health programs are culturally competent and responsive to the needs of diverse populations. Public health institutions are increasingly focusing on recruiting and retaining a diverse workforce, as well as providing training on cultural competence and health equity.
- Global Health Education: As public health becomes increasingly globalized, there is a growing emphasis on global health education. Public health programs are incorporating global health perspectives into their curricula, providing students with the knowledge and skills needed to address health challenges on a global scale.
Conclusion
The field of public health is undergoing significant transformation, driven by emerging trends and challenges that are reshaping the way public health is practiced and perceived. From the integration of digital health technologies and precision public health to the growing focus on mental health, climate change, health equity, and pandemic preparedness, these trends are setting the stage for a new era in public health.
As public health continues to evolve, it is essential that public health professionals remain adaptable, innovative, and committed to addressing the complex and interconnected health challenges facing societies today. By embracing these trends and leading changes in public health, we can create a healthier, more equitable, and resilient future for all.

-
 Press Release4 days ago
Press Release4 days agoClinical Trials Market Set for Robust Growth, Driven by Drug Development Surge and Digital Innovation
-

 Press Release5 days ago
Press Release5 days agoFill-Finish Pharmaceutical Contract Manufacturing Market Expected to Flourish Amid Biopharmaceutical Boom and Global Outsourcing Trend by 2035
-

 Business6 days ago
Business6 days agoHow Managed IT Solutions Help Small Teams Compete at Enterprise Scale
-
 Press Release5 days ago
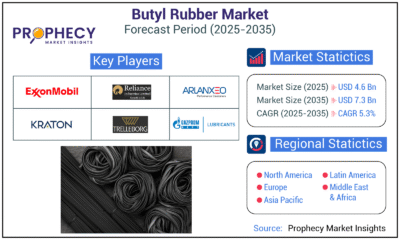
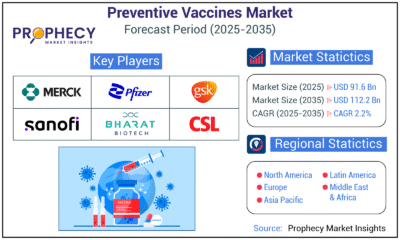
Press Release5 days agoGreen Bio Chemicals Market Poised for Sustainable Growth amidst Global Shift to Eco-Friendly Alternatives by 2035
-
 Press Release5 days ago
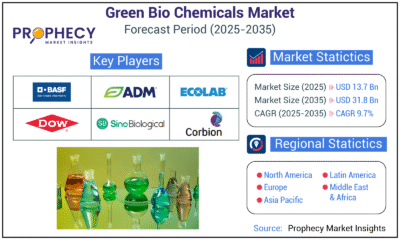
Press Release5 days agoIndustrial Boiler Market Expected to Surpass USD 24.4 Billion by 2035 Amid Growing Demand for Energy Efficiency and Industrialization
-
 Press Release5 days ago
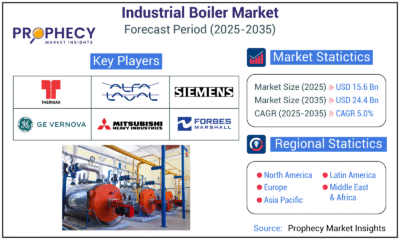
Press Release5 days agoPreventive Vaccines Market to Witness Strong Growth by 2035
-

 Press Release5 days ago
Press Release5 days agoPet Food Nutraceutical Market Set for Robust Expansion Amid Rising Demand for Pet Wellness by 2035
-

 Press Release4 days ago
Press Release4 days agoWaterproof Structural Adhesives Market: A Comprehensive Study Towards USD 10.3 Billion in 2035





























