Mental Health
Mental Health Stigma: Breaking Down Barriers to Treatment

Mental health is an essential component of overall well-being, influencing how individuals think, feel, and behave. Despite its critical importance, society has historically marginalized mental health issues, treating them as taboo subjects unworthy of open discussion or attention. This neglect has led to widespread stigma, fostering misconceptions and prejudices that deter people from seeking help when they need it most. The stigma surrounding mental health can be as damaging as the conditions themselves, creating a ripple effect that impacts individuals, families, and entire communities.
Mental health stigma is a formidable barrier to treatment and wellness, impeding progress in addressing the global mental health crisis. Over the years, efforts to break down this stigma have gained momentum, but much work remains to be done. This article explores the origins and consequences of mental health stigma, delves into the various forms it takes, and highlights the ongoing efforts to break down barriers to treatment, promoting a more inclusive and supportive society.
1. The Roots of Mental Health Stigma
Mental health stigma has deep historical and cultural roots, often fueled by misunderstanding and fear. In ancient times, mental illness was commonly attributed to supernatural forces, such as demonic possession or divine punishment. The afflicted were ostracized, mistreated, and sometimes subjected to brutal and inhumane treatments, including exorcisms, bloodletting, and confinement in asylums.
During the Middle Ages, mental illness was often viewed as a moral failing or a sign of personal weakness. Those struggling with mental health issues were labeled as “mad” or “insane” and frequently faced imprisonment, physical abuse, or abandonment. These harsh attitudes persisted for centuries, reinforced by cultural and religious beliefs that stigmatized those with mental health conditions.
In the 19th and early 20th centuries, the rise of psychiatry brought some progress in understanding mental illness, but stigma remained entrenched. Psychiatric institutions, or “lunatic asylums,” often served as places of confinement rather than treatment, perpetuating the notion that people with mental health disorders were dangerous and unpredictable. These institutions isolated individuals from society, further deepening the divide between the mentally ill and the general population.
The 20th century saw significant advancements in the understanding and treatment of mental health conditions, including the development of psychoanalysis, psychotropic medications, and cognitive behavioral therapies. However, the stigma associated with mental illness continued to thrive, largely due to lingering misconceptions, media portrayals, and societal norms that viewed mental health as a private matter, not to be openly discussed or acknowledged.
2. Types of Mental Health Stigma
Stigma surrounding mental health takes various forms, each of which contributes to the overall societal bias against individuals living with mental health conditions. Understanding these forms of stigma is essential in devising strategies to combat them.
- Public Stigma
Public stigma refers to the negative attitudes and beliefs that the general population holds about individuals with mental health conditions. This form of stigma is perpetuated by stereotypes that portray people with mental illness as dangerous, incompetent, or morally flawed. These stereotypes are often reinforced by sensationalized media coverage, which tends to focus on extreme cases of violence or erratic behavior associated with mental illness, further entrenching fear and prejudice.
For instance, news reports that link mental illness with violent crime disproportionately contribute to the public perception that individuals with conditions such as schizophrenia or bipolar disorder are a threat to society. In reality, the vast majority of people with mental health conditions are not violent, and they are more likely to be victims of violence than perpetrators. Nevertheless, public stigma persists, shaping how individuals with mental illness are treated in social, professional, and legal settings.
- Self-Stigma
Self-stigma occurs when individuals internalize the negative stereotypes and prejudices associated with mental illness. Those who experience self-stigma may feel ashamed, guilty, or unworthy, leading them to avoid seeking help or disclosing their condition to others. Self-stigma can be particularly damaging, as it undermines an individual’s sense of self-worth and can exacerbate symptoms of anxiety, depression, and other mental health conditions.
For example, a person struggling with depression may believe they are “weak” for feeling overwhelmed or unable to cope with life’s challenges. This internalized shame can prevent them from reaching out for support, delaying treatment and prolonging their suffering. Self-stigma also contributes to isolation, as individuals may withdraw from social interactions out of fear of being judged or rejected.
- Structural Stigma
Structural stigma refers to the institutional policies and practices that discriminate against individuals with mental health conditions. This form of stigma is deeply embedded in societal systems, including healthcare, employment, and the legal system. Structural stigma can create significant barriers to accessing mental health care, securing stable employment, and receiving fair treatment under the law.
In healthcare, structural stigma may manifest as limited funding for mental health services, inadequate training for healthcare providers, or restrictive insurance policies that make mental health treatment unaffordable or inaccessible. In the workplace, individuals with mental health conditions may face discrimination in hiring, promotions, or job retention, as employers may view them as less capable or reliable. In the legal system, people with mental health conditions may be more likely to face harsher penalties, less access to legal representation, or inadequate mental health care while incarcerated.
- Cultural Stigma
Cultural stigma refers to the unique ways in which different societies and communities view and respond to mental health conditions. Cultural beliefs, traditions, and values can significantly influence how mental illness is perceived and treated. In some cultures, mental health issues may be seen as a source of shame or dishonor, leading families to conceal a relative’s condition or avoid seeking help altogether. In other cultures, mental illness may be viewed as a spiritual or supernatural problem, requiring intervention by religious leaders rather than mental health professionals.
Cultural stigma can also affect how mental health symptoms are expressed and interpreted. For example, in some cultures, individuals may be more likely to report physical symptoms (such as headaches or fatigue) rather than emotional symptoms (such as sadness or anxiety), which can complicate diagnosis and treatment. Understanding cultural stigma is essential in providing culturally competent care and developing interventions that are sensitive to the diverse needs of different populations.
3. The Impact of Stigma on Mental Health Treatment
The consequences of mental health stigma are far-reaching, affecting not only individuals with mental health conditions but also their families, communities, and society as a whole. Stigma creates significant barriers to treatment, which can lead to worsening symptoms, increased disability, and higher mortality rates. Below are some of the key ways in which stigma impacts mental health treatment:
- Delay in Seeking Treatment
One of the most pervasive effects of mental health stigma is the delay in seeking treatment. Many individuals avoid seeking help due to fear of being judged, labeled, or ostracized. Research has shown that people with mental health conditions often wait years, or even decades, before seeking treatment, during which time their symptoms may worsen and become more difficult to manage.
For example, individuals with depression or anxiety may delay seeking help because they believe they should be able to “snap out of it” or “tough it out” on their own. Others may worry that admitting to a mental health issue will harm their reputation, relationships, or career prospects. This delay in treatment not only prolongs suffering but can also lead to more severe mental health crises, including hospitalization, self-harm, or suicide.
- Inadequate Access to Care
Stigma also contributes to disparities in access to mental health care. Structural stigma, in particular, creates systemic barriers that make it difficult for individuals to access the care they need. In many countries, mental health services are underfunded, leading to long wait times, limited availability of specialists, and inadequate support for those in crisis.
For marginalized populations, such as racial and ethnic minorities, LGBTQ+ individuals, and low-income communities, the barriers to accessing mental health care are often even greater. These groups may face additional layers of discrimination, cultural stigma, or logistical challenges (such as lack of transportation or insurance) that further limit their ability to receive appropriate care.
- Non-Compliance with Treatment
Even when individuals do seek treatment, stigma can impact their willingness to adhere to prescribed treatment plans. Fear of being labeled “crazy” or “unstable” may lead individuals to discontinue medication, skip therapy sessions, or avoid disclosing their full symptoms to healthcare providers. This non-compliance can undermine the effectiveness of treatment, leading to relapse or worsening of symptoms.
In some cases, individuals may also be reluctant to engage in certain types of treatment, such as psychotherapy, due to cultural stigma or misconceptions about its value. For example, in cultures that place a high value on self-reliance, individuals may view seeking help from a therapist as a sign of weakness or failure.
- Social Isolation
Stigma can also lead to social isolation, as individuals with mental health conditions may withdraw from friends, family, and community activities out of fear of being judged or rejected. This isolation can exacerbate feelings of loneliness, depression, and anxiety, creating a vicious cycle that further hinders recovery.
Social isolation can also have practical consequences, such as reducing access to informal support networks that might otherwise provide emotional, financial, or logistical assistance. For example, a person who feels too ashamed to disclose their mental health condition to their employer may struggle to take time off for therapy appointments or manage their workload during periods of acute stress.
- Discrimination and Inequality
Stigma also perpetuates discrimination and inequality in various aspects of life, including education, employment, housing, and the criminal justice system. Individuals with mental health conditions are more likely to face barriers in accessing quality education, securing stable employment, and obtaining adequate housing. Discrimination in these areas can contribute to a cycle of poverty, homelessness, and incarceration, further marginalizing people with mental health conditions and limiting their opportunities for recovery and reintegration into society.
In the workplace, for instance, individuals with mental health conditions may be passed over for promotions, denied reasonable accommodations, or unfairly terminated. This discrimination not only affects the individual’s financial stability but also reinforces the stigma that people with mental illness are less capable or productive than their peers.
4. Breaking Down the Barriers: Efforts to Combat Mental Health Stigma
While the challenges posed by mental health stigma are significant, there is growing recognition of the need to address this issue on multiple fronts. Breaking down the barriers to mental health treatment requires a comprehensive approach that involves individuals, communities, healthcare systems, and policymakers. Below are some of the key strategies and initiatives aimed at combating mental health stigma and promoting greater access to care.
- Public Awareness Campaigns
Public awareness campaigns are one of the most effective tools for challenging stereotypes and changing societal attitudes about mental health. These campaigns aim to educate the public about the realities of mental illness, dispel myths, and encourage empathy and understanding. By highlighting personal stories of individuals living with mental health conditions, these campaigns humanize the issue and reduce fear and prejudice.
One example of a successful public awareness campaign is the “Time to Change” initiative in the United Kingdom, which has focused on reducing stigma through social media, public events, and partnerships with schools, employers, and healthcare providers. The campaign encourages open conversations about mental health and has contributed to measurable reductions in public stigma over time.
- Mental Health Education in Schools
Integrating mental health education into school curricula is another critical strategy for combating stigma and promoting early intervention. By teaching young people about mental health, emotional well-being, and coping strategies, schools can help reduce the stigma that often surrounds these topics and empower students to seek help when needed.
Mental health education programs can also promote resilience and emotional intelligence, equipping students with the skills to manage stress, build healthy relationships, and navigate life’s challenges. These programs are particularly effective when they involve peer support and mentorship, as young people are often more comfortable discussing mental health issues with their peers than with adults.
- Workplace Mental Health Initiatives
Workplaces play a crucial role in shaping attitudes toward mental health, as employment is a significant part of most people’s lives. Employers can help combat stigma by creating supportive and inclusive work environments that prioritize employee well-being. This can include offering mental health benefits, providing access to counseling services, implementing flexible work arrangements, and training managers to recognize and respond to signs of mental health issues among their employees.
Workplace mental health initiatives not only benefit employees but also contribute to improved productivity, reduced absenteeism, and lower healthcare costs for employers. Research has shown that companies that invest in mental health support see a positive return on investment, making it a win-win for both employers and employees.
- Policy and Advocacy Efforts
Advocacy efforts at the local, national, and international levels are essential for addressing the structural and systemic barriers that contribute to mental health stigma. Policymakers play a key role in shaping mental health care systems, funding services, and enacting anti-discrimination laws that protect the rights of individuals with mental health conditions.
In recent years, there have been significant strides in mental health policy reform in many countries. For example, the Mental Health Parity and Addiction Equity Act in the United States requires insurance companies to provide equal coverage for mental health and substance use treatment, helping to reduce financial barriers to care. Similarly, the World Health Organization’s Mental Health Action Plan (2013-2020) has focused on improving access to mental health services and promoting human rights for individuals with mental health conditions worldwide.
- Peer Support and Community Programs
Peer support programs, in which individuals with lived experience of mental health conditions provide support and guidance to others, have proven to be an effective way to combat stigma and promote recovery. These programs offer a safe and non-judgmental space for individuals to share their experiences, learn coping strategies, and connect with others who understand their challenges.
Community-based mental health programs also play a vital role in breaking down stigma, particularly in underserved or marginalized communities. These programs often work in partnership with local organizations, religious institutions, and cultural leaders to provide culturally sensitive care and education, helping to reduce the stigma associated with mental illness in diverse populations.
5. The Road Ahead: A Vision for a Stigma-Free Future
While progress has been made in reducing mental health stigma, significant challenges remain. To create a stigma-free future, it is essential to continue raising awareness, promoting education, and advocating for policies that prioritize mental health. A comprehensive approach that addresses the individual, societal, and structural dimensions of stigma is needed to ensure that everyone, regardless of their mental health status, has access to the care and support they need.
Breaking down the barriers to mental health treatment is not only a matter of justice and equity but also a moral imperative. Mental health is a fundamental human right, and no one should be denied the opportunity to live a fulfilling and meaningful life due to stigma or discrimination. By working together with individuals, communities, healthcare providers, policymakers, and advocates we can create a world where mental health is treated with the same dignity and respect as physical health, and where everyone has the chance to thrive.
-
 Press Release5 days ago
Press Release5 days agoClinical Trials Market Set for Robust Growth, Driven by Drug Development Surge and Digital Innovation
-

 Press Release5 days ago
Press Release5 days agoFill-Finish Pharmaceutical Contract Manufacturing Market Expected to Flourish Amid Biopharmaceutical Boom and Global Outsourcing Trend by 2035
-
 Press Release5 days ago
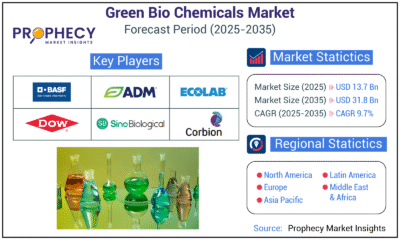
Press Release5 days agoGreen Bio Chemicals Market Poised for Sustainable Growth amidst Global Shift to Eco-Friendly Alternatives by 2035
-

 Business6 days ago
Business6 days agoHow Managed IT Solutions Help Small Teams Compete at Enterprise Scale
-
 Press Release5 days ago
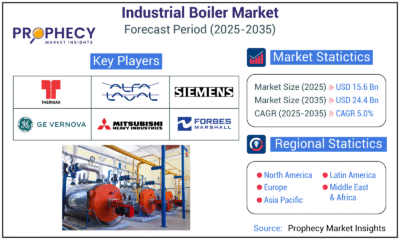
Press Release5 days agoIndustrial Boiler Market Expected to Surpass USD 24.4 Billion by 2035 Amid Growing Demand for Energy Efficiency and Industrialization
-
 Press Release5 days ago
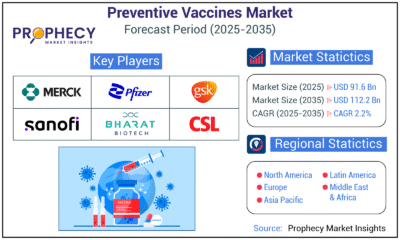
Press Release5 days agoPreventive Vaccines Market to Witness Strong Growth by 2035
-

 Press Release5 days ago
Press Release5 days agoPet Food Nutraceutical Market Set for Robust Expansion Amid Rising Demand for Pet Wellness by 2035
-

 Press Release5 days ago
Press Release5 days agoWaterproof Structural Adhesives Market: A Comprehensive Study Towards USD 10.3 Billion in 2035