Healthcare
Food Allergies and Intolerances: Managing Reactions and Living Well

Food allergies and intolerances are widespread and often misunderstood conditions that affect millions globally, with significant impacts on quality of life. Understanding the distinctions between the two, along with effective management strategies, is essential for those affected and their families. In this report, we will explore the latest data, management strategies, and living solutions for individuals facing food allergies and intolerances, drawing from current research and expert guidelines.
Understanding the Differences Between Food Allergies and Intolerances
Food allergies and intolerances, while often used interchangeably, are distinct conditions involving different physiological mechanisms. A food allergy is an immune system response to a specific protein found in foods. The immune system mistakes this protein as harmful and releases antibodies to fight it, leading to symptoms that range from mild (e.g., rashes and hives) to severe (e.g., anaphylaxis). Anaphylaxis, a life-threatening reaction, can include swelling of the airways, a drop in blood pressure, and even death if untreated. Common allergens include peanuts, tree nuts, shellfish, milk, eggs, soy, wheat, and fish. These reactions can occur within minutes of exposure and require immediate intervention, often with epinephrine auto-injectors.
In contrast, a food intolerance does not involve the immune system but occurs when the body struggles to digest certain foods. The most common example is lactose intolerance, where the body lacks the enzyme lactase, required to break down lactose, the sugar in milk. This leads to gastrointestinal symptoms like bloating, gas, and diarrhea. Other common intolerances involve substances like gluten (celiac disease), sulfites in wine, or chemical additives like monosodium glutamate (MSG). Unlike allergies, intolerances generally require larger amounts of the offending food to trigger symptoms.
Prevalence and Trends
The incidence of food allergies and intolerances is rising globally. In the United States, food allergies affect approximately 32 million people, including 1 in 13 children. This represents a growing public health challenge, particularly in schools, where accidental exposure to allergens can pose serious risks. Food intolerances are also common, with lactose intolerance affecting up to 68% of the global population, particularly in regions like East Asia and parts of Africa where dairy consumption is historically lower.
Moreover, certain food allergies, such as those to peanuts and tree nuts, are becoming more common, possibly due to changing environmental factors and modern dietary habits. In response, many countries have introduced allergen labeling laws and school safety protocols to mitigate risks.
Managing Reactions: Tools and Techniques
For individuals with food allergies, prevention is the primary strategy. This involves strict avoidance of allergenic foods and careful label reading. The U.S. Food Allergen Labeling and Consumer Protection Act (FALCPA) mandates that foods containing common allergens such as peanuts, shellfish, and dairy must be clearly labeled. Moreover, individuals with severe allergies are often advised to carry epinephrine auto-injectors (e.g., EpiPen) at all times. In case of exposure, administering epinephrine can reverse the symptoms of anaphylaxis, and seeking immediate medical help is crucial.
Oral Immunotherapy (OIT) is an emerging treatment for certain allergies, particularly peanut allergies. This involves gradually exposing the allergic individual to increasing amounts of the allergen to desensitize the immune response. OIT has shown promise in reducing the severity of allergic reactions, though it is not a cure and requires close medical supervision.
For food intolerances, management often involves dietary adjustments rather than emergency interventions. Lactase supplements, for instance, can help people with lactose intolerance digest dairy products, while those with gluten intolerance must follow a gluten-free diet. Many people with food intolerances rely on substitution strategies, such as using almond or soy milk instead of dairy, or gluten-free grains like quinoa and rice instead of wheat.
Daily Living with Food Allergies and Intolerances
Living with food allergies or intolerances can be challenging, especially in social settings like restaurants, schools, and family gatherings. However, with the right precautions, people can lead fulfilling lives while managing their conditions.
Dining Out Safely: One of the most significant challenges for people with food allergies is eating outside the home. Restaurants may inadvertently cross-contaminate food or fail to disclose allergens. To address this, individuals are encouraged to communicate clearly with restaurant staff about their allergies. Some restaurants now include allergen-friendly menus, and mobile apps such as Spokin help users find allergy-safe dining options.
School and Work Accommodations: Schools, workplaces, and public institutions are increasingly implementing allergen-free zones and protocols. In schools, many have adopted peanut-free policies, while some have designated lunch areas for children with severe allergies to reduce the risk of exposure.
Mental Health and Well-Being: Living with food allergies and intolerances can take a psychological toll, especially for children and teenagers who may feel isolated or anxious. Research has shown that up to 30% of children with food allergies experience higher levels of anxiety compared to their peers. Support groups and therapy can be valuable resources, helping individuals manage the emotional stress of living with these conditions.
Family Support and Education: Families play a crucial role in managing food allergies and intolerances. It’s essential for all members to understand the risks and how to prevent exposure. Parents often need to work closely with schools, daycares, and caregivers to ensure safety protocols are followed. FARE (Food Allergy Research & Education) and other organizations provide educational resources and community support to help families navigate these challenges.
Future Directions: Advances in Treatment and Policy
The landscape of food allergy management is evolving with new research and technologies. Scientists are investigating biologic therapies, such as omalizumab, that could help reduce the severity of allergic reactions by modulating the immune system. In 2023, the U.S. FDA approved Xolair as the first treatment to reduce the risk of food allergy reactions when used alongside oral immunotherapy.
Moreover, advocacy groups are pushing for stronger allergen labeling laws and improved access to life-saving medications like epinephrine. Cost remains a barrier for many families, with epinephrine auto-injectors costing hundreds of dollars. Some organizations are lobbying for affordable epinephrine options and increased coverage under health insurance.
Conclusion
Food allergies and intolerances present unique challenges, but with proper management strategies, individuals can live well and avoid serious health risks. As awareness continues to grow, improvements in medical treatments, dietary accommodations, and public policies are making life safer and more comfortable for those affected. Whether through careful avoidance of allergens, use of new immunotherapy techniques, or advocating for better labeling and affordability, the future of food allergy and intolerance management looks promising.
-

 Press Release5 days ago
Press Release5 days agoBellarium ($BEL) Price Prediction: Could It Hit $5 by 2026?
-
 Press Release2 days ago
Press Release2 days agoClinical Trials Market Set for Robust Growth, Driven by Drug Development Surge and Digital Innovation
-
 Press Release3 days ago
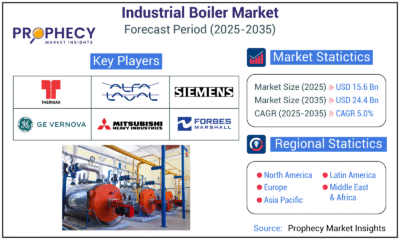
Press Release3 days agoIndustrial Boiler Market Expected to Surpass USD 24.4 Billion by 2035 Amid Growing Demand for Energy Efficiency and Industrialization
-
 Press Release3 days ago
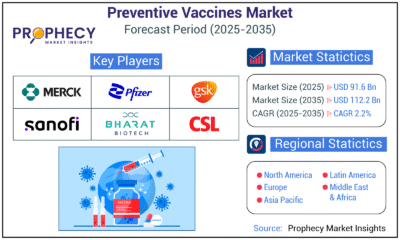
Press Release3 days agoPreventive Vaccines Market to Witness Strong Growth by 2035
-

 Business4 days ago
Business4 days agoHow Managed IT Solutions Help Small Teams Compete at Enterprise Scale
-
 Press Release3 days ago
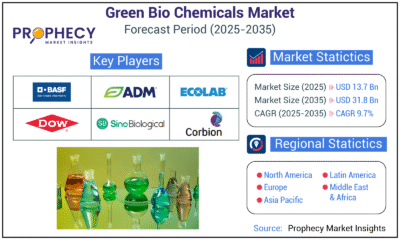
Press Release3 days agoGreen Bio Chemicals Market Poised for Sustainable Growth amidst Global Shift to Eco-Friendly Alternatives by 2035
-

 Press Release3 days ago
Press Release3 days agoFill-Finish Pharmaceutical Contract Manufacturing Market Expected to Flourish Amid Biopharmaceutical Boom and Global Outsourcing Trend by 2035
-

 Press Release3 days ago
Press Release3 days agoPet Food Nutraceutical Market Set for Robust Expansion Amid Rising Demand for Pet Wellness by 2035