Health & Fitness
Core Principles of Protecting Health in Diverse Environments: A Comprehensive Guide

Health protection in diverse environments is a complex and multifaceted endeavor that necessitates a nuanced understanding of various social, economic, cultural, and environmental factors. As the global landscape continues to evolve, with increasing urbanization, climate change, and population mobility, the need to protect health in diverse settings becomes ever more critical. This comprehensive guide explores the core principles of safeguarding health across different environments, emphasizing the importance of adaptability, equity, community engagement, and evidence-based practices.
Understanding Diverse Environments
“Diverse environments” refers to the wide range of physical, social, and cultural settings where people live, work, and interact. These environments can be classified into several categories, each presenting unique challenges and opportunities for health protection:
- Urban and Rural Settings: Urban environments are characterized by high population density, advanced infrastructure, and greater access to healthcare services. However, they also face pollution, stress, and social isolation. On the other hand, rural environments often have limited access to healthcare and fewer resources and may face challenges like inadequate sanitation and poor infrastructure.
- High-Income and Low-Income Regions: High-income regions typically have better healthcare systems, higher literacy rates, and more robust public health infrastructure. In contrast, low-income areas may struggle with inadequate healthcare, malnutrition, infectious diseases, and poor living conditions, exacerbated by limited resources and governmental support.
- Culturally Diverse Communities: Health protection in culturally diverse environments requires sensitivity to different cultural practices, beliefs, and languages. Understanding cultural context is crucial for effective health interventions and ensuring community buy-in.
- Disaster-Prone and Conflict Zones: Environments affected by natural disasters or conflicts pose significant challenges to health protection. These settings often experience disruptions in healthcare delivery, sanitation, and access to clean water, leading to heightened risks of disease outbreaks and long-term health consequences.
- Climate-Impacted Regions: Areas heavily impacted by climate change face unique health challenges, including increased frequency of extreme weather events, changes in disease patterns, and population displacement. Climate change exacerbates existing vulnerabilities, making health protection more complex.
Core Principles of Health Protection in Diverse Environments
Protecting health in diverse environments requires a multi-dimensional approach that integrates various principles to address the unique challenges of different settings. Below are the core principles that guide effective health protection strategies:
1) Equity and Social Justice
Equity is at the heart of health protection. It ensures that all individuals, regardless of socioeconomic status, ethnicity, or geographic location, have access to the resources they need to achieve good health. Social justice emphasizes addressing inequalities and ensuring health resources and services are fair.
- Addressing Disparities: Health protection strategies must identify and address disparities in health outcomes, particularly in marginalized and vulnerable populations. This includes tackling barriers to healthcare access, such as cost, transportation, and discrimination.
- Inclusive Health Policies: Policymakers must ensure that health policies are inclusive and cater to the needs of all community members, particularly those who are often overlooked, such as indigenous populations, migrants, and people with disabilities.
- Community-Centered Approaches: Engaging communities in developing and implementing health protection strategies is crucial for ensuring that interventions are relevant, culturally appropriate, and sustainable.
2) Adaptability and Resilience
Health protection strategies must be adaptable to the changing dynamics of diverse environments. Resilience, the ability to withstand and recover from health threats, is equally important.
- Flexible Health Systems: Health systems must be designed to adapt to new challenges, such as emerging infectious diseases, climate change, and technological advancements. This requires continuous monitoring, evaluation, and the capacity to implement rapid changes when necessary.
- Emergency Preparedness: Preparedness for emergencies, whether natural disasters, disease outbreaks, or conflicts, is essential. This involves developing robust contingency plans, training healthcare workers, and ensuring that basic supplies and resources are available.
- Sustainable Practices: Protecting health in diverse environments requires long-term sustainability. This includes investing in healthcare infrastructure, training, and research to withstand future challenges.
3) Prevention and Health Promotion
Prevention and health promotion are foundational to health protection. Preventing diseases and promoting healthy behaviors can significantly reduce the burden on healthcare systems and improve overall health outcomes.
- Vaccination Programs: Immunization is among the most effective public health interventions. Ensuring high vaccination coverage across different populations and settings is crucial for preventing the spread of infectious diseases.
- Health Education: Educating communities about healthy behaviors, such as proper nutrition, physical activity, and hygiene practices, empower individuals to take control of their health and prevent diseases.
- Environmental Health: Addressing environmental factors contributing to ill health, such as pollution, unsafe water, and inadequate sanitation, is critical for disease prevention and health promotion.
4) Evidence-Based Practices
Evidence-based practices are essential for adequately protecting health in diverse environments. These practices involve using the best evidence to guide decision-making and health interventions.
- Data Collection and Research: Robust data collection and research are necessary to understand health trends, identify emerging health threats, and evaluate the effectiveness of health interventions. This information should inform policy and practice.
- Monitoring and Evaluation: Continuous monitoring and evaluation of health programs and policies ensure that they are effective, efficient, and responsive to the population’s needs.
- Integration of Traditional and Modern Medicine: In culturally diverse environments, integrating traditional medicine practices with modern healthcare can enhance the effectiveness of health interventions. This requires respect for local knowledge and practices and collaboration between traditional healers and healthcare professionals.
5) Intersectoral Collaboration
Protecting health in diverse environments is not the sole responsibility of the health sector. Intersectoral collaboration is essential, involving multiple sectors such as education, agriculture, housing, and transportation.
- Collaborative Governance: Governments should foster collaboration between different sectors to address the social determinants of health, such as poverty, education, and housing. This holistic approach ensures comprehensive health protection strategies address the root causes of ill health.
- Public-Private Partnerships: Partnerships between public and private sectors can enhance the delivery of health services, particularly in resource-limited settings. These partnerships can mobilize additional resources, expertise, and innovation.
- Global Cooperation: Health protection in diverse environments often requires international collaboration, particularly in addressing global health threats like pandemics and climate change. Global cooperation ensures the sharing of knowledge, resources, and technologies across borders.
6) Ethical Considerations
Ethical considerations are paramount in protecting health, especially in diverse environments where cultural practices, values, and beliefs may differ significantly.
- Informed Consent: Informed consent is crucial in all health interventions. This involves ensuring that individuals understand the risks and benefits of a health intervention and have the autonomy to make decisions about their health.
- Cultural Sensitivity: Health protection strategies must be culturally sensitive, respecting the beliefs, practices, and traditions of different communities. This requires cultural competence among healthcare providers and the inclusion of cultural leaders in health planning.
- Transparency and Accountability: Health authorities and organizations must be transparent in their decision-making processes and accountable for their actions. This builds trust with communities and ensures that health protection strategies are ethical and just.
7) Technology and Innovation
Technology and innovation play a critical role in advancing health protection in diverse environments. From digital health tools to new medical technologies, innovation can enhance the reach, efficiency, and effectiveness of health interventions.
- Telemedicine and E-Health: Telemedicine and e-health platforms can bridge the gap in healthcare access, particularly in remote and underserved areas. These technologies enable healthcare providers to deliver care across distances, monitor patients remotely, and provide timely health information.
- Data Analytics and Artificial Intelligence: The use of data analytics and artificial intelligence (AI) in health protection can improve disease surveillance, predict outbreaks, and personalize health interventions. These tools can also enhance the efficiency of healthcare systems by optimizing resource allocation and decision-making.
- Innovative Health Financing: Innovative financing models, such as health savings accounts, microinsurance, and outcome-based financing, can improve access to healthcare and ensure financial sustainability in diverse environments.
8) Environmental Stewardship
Environmental stewardship is an integral component of health protection, particularly in the context of climate change and environmental degradation. Protecting the environment is essential for ensuring long-term health and well-being.
- Sustainable Development: Health protection strategies should be aligned with sustainable development goals (SDGs), ensuring that health interventions do not compromise the environment. This includes promoting renewable energy, reducing waste, and protecting natural resources.
- Climate Change Mitigation: Addressing the health impacts of climate change requires proactive measures to reduce greenhouse gas emissions, protect vulnerable populations from extreme weather events, and promote climate-resilient health systems.
- Biodiversity Conservation: Protecting biodiversity is essential for maintaining the ecological balance and ensuring the availability of resources such as clean water, food, and medicine. Health protection strategies should include efforts to conserve natural habitats and protect endangered species.
9) Community Engagement and Empowerment
Engaging and empowering communities is crucial for the success of health protection strategies. Communities play a vital role in identifying health needs, implementing interventions, and sustaining health improvements.
- Participatory Approaches: Health protection strategies should involve communities in decision-making processes, ensuring that interventions are relevant, acceptable, and effective. Participatory approaches foster ownership and accountability among community members.
- Capacity Building: Empowering communities through capacity building enhances their ability to protect their health and respond to health threats. This includes training community health workers, providing health education, and supporting local health initiatives.
- Social Mobilization: Social mobilization efforts, such as awareness campaigns and advocacy, can galvanize communities to take collective action on health issues. This is particularly important in addressing public health challenges such as vaccination, sanitation and disease prevention.
10) Ethical Research and Innovation
In the pursuit of advancing health protection, it is essential to conduct research and innovation in an ethical manner. Ethical research ensures that the rights and dignity of individuals and communities are respected and that the benefits of research are equitably distributed.
- Ethical Approval: All research involving human subjects must undergo rigorous ethical review and approval processes. This ensures that research is conducted with respect for participants’ autonomy, confidentiality, and well-being.
- Community Involvement in Research: Involving communities in the research process, from design to implementation and dissemination, ensures that research addresses local needs and respects cultural contexts.
- Benefit Sharing: The benefits of research and innovation should be shared equitably with the communities involved. This includes access to new technologies, healthcare improvements, and capacity-building opportunities.
Conclusion
Protecting health in diverse environments is a complex but vital task that requires a holistic, adaptable, and ethical approach. The core principles outlined in this guide; equity, adaptability, prevention, evidence-based practices, intersectoral collaboration, ethical considerations, technology and innovation, environmental stewardship, community engagement, and ethical research provide a comprehensive framework for addressing the unique challenges of health protection in diverse settings.
As the world continues to face new health challenges, from pandemics to climate change, it is imperative that health protection strategies are inclusive, sustainable, and responsive to the needs of all populations. By adhering to these core principles, we can ensure that health protection efforts are effective, equitable, and resilient, ultimately leading to improved health outcomes for people in all environments.
-
 Press Release4 days ago
Press Release4 days agoClinical Trials Market Set for Robust Growth, Driven by Drug Development Surge and Digital Innovation
-

 Press Release5 days ago
Press Release5 days agoFill-Finish Pharmaceutical Contract Manufacturing Market Expected to Flourish Amid Biopharmaceutical Boom and Global Outsourcing Trend by 2035
-

 Business6 days ago
Business6 days agoHow Managed IT Solutions Help Small Teams Compete at Enterprise Scale
-
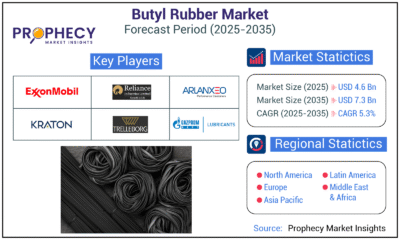
 Press Release5 days ago
Press Release5 days agoGreen Bio Chemicals Market Poised for Sustainable Growth amidst Global Shift to Eco-Friendly Alternatives by 2035
-
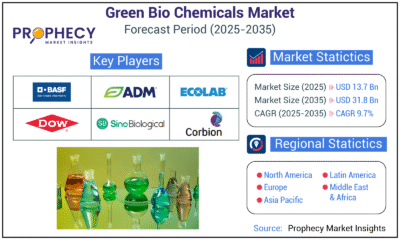
 Press Release5 days ago
Press Release5 days agoIndustrial Boiler Market Expected to Surpass USD 24.4 Billion by 2035 Amid Growing Demand for Energy Efficiency and Industrialization
-
 Press Release5 days ago
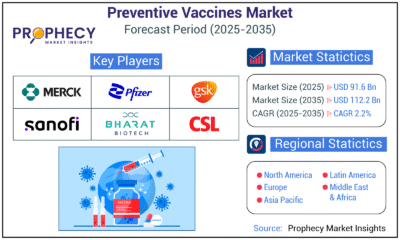
Press Release5 days agoPreventive Vaccines Market to Witness Strong Growth by 2035
-

 Press Release5 days ago
Press Release5 days agoPet Food Nutraceutical Market Set for Robust Expansion Amid Rising Demand for Pet Wellness by 2035
-

 Press Release4 days ago
Press Release4 days agoWaterproof Structural Adhesives Market: A Comprehensive Study Towards USD 10.3 Billion in 2035