Healthcare
Chronic Fatigue Syndrome: Understanding and Managing Symptoms
Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME), is a complex and debilitating disorder characterized by extreme fatigue that is not alleviated by rest and is not directly caused by other medical conditions. This condition can severely impact a person’s ability to perform everyday activities, often leading to a significant decline in quality of life. Despite affecting millions of people worldwide, CFS/ME is still poorly understood and frequently misunderstood. In this article, we will explore the intricacies of Chronic Fatigue Syndrome, including its potential causes, symptoms, diagnostic challenges, and management strategies.
Understanding Chronic Fatigue Syndrome
CFS/ME is more than just feeling tired. It is a multifaceted illness affecting various body systems, including the immune, nervous, and endocrine systems. The hallmark symptom of CFS is persistent and unexplained fatigue that lasts for at least six months and is accompanied by a variety of other symptoms, such as sleep disturbances, cognitive impairment, and post-exertional malaise (PEM).
- Defining the Illness
Chronic Fatigue Syndrome was first recognized in the 1980s, but references to similar conditions date back centuries. It is characterized by profound and disabling fatigue, lasting for more than six months and not attributable to exertion or other medical conditions. The fatigue is so severe that it impairs the individual’s ability to engage in daily activities.
- Terminology and Controversy
The term “Chronic Fatigue Syndrome” has been a source of controversy within the medical community, as some feel it trivializes the severity of the condition. Myalgic Encephalomyelitis (ME) is another term often used interchangeably, though it emphasizes inflammation of the brain and spinal cord. The term ME/CFS is increasingly used to capture the complex nature of the disorder. In 2015, the Institute of Medicine (now the National Academy of Medicine) proposed a new name, Systemic Exertion Intolerance Disease (SEID), which highlights the key feature of post-exertional malaise.
Symptoms of Chronic Fatigue Syndrome
The symptoms of CFS/ME are varied and can fluctuate in severity from day to day. The most common symptoms include:
- Extreme Fatigue
The most prominent symptom of CFS/ME is a profound fatigue that is not relieved by rest or sleep. This fatigue is often described as a feeling of overwhelming exhaustion and can be exacerbated by physical or mental exertion. Unlike normal tiredness, this fatigue is not proportional to activity levels and can be debilitating.
- Post-Exertional Malaise (PEM)
PEM is a hallmark of CFS/ME, where symptoms worsen after physical or mental exertion. Activities that would not normally cause fatigue, such as light exercise or mental tasks, can trigger a relapse of symptoms that may last for days or even weeks. This phenomenon makes managing daily activities challenging for individuals with CFS/ME.
- Cognitive Impairment
Often referred to as “brain fog,” cognitive impairment in CFS/ME can manifest as difficulties with concentration, memory, and information processing. This can impact an individual’s ability to work, study, or perform tasks that require mental effort.
- Sleep Disturbances
Despite experiencing overwhelming fatigue, many individuals with CFS/ME report sleep disturbances such as insomnia, unrefreshing sleep, or disrupted sleep patterns. This can exacerbate other symptoms and contribute to the overall feeling of unwellness.
- Pain
Many individuals with CFS/ME experience widespread pain, including muscle aches, joint pain, and headaches. Unlike other conditions, the pain is not due to inflammation or injury but is thought to be related to abnormalities in pain processing by the central nervous system.
- Orthostatic Intolerance
Orthostatic intolerance, or difficulty remaining upright, is another common symptom. It includes conditions such as Postural Orthostatic Tachycardia Syndrome (POTS), where there is an abnormal increase in heart rate upon standing, leading to dizziness, lightheadedness, or fainting.
- Sensitivity to External Stimuli
Individuals with CFS/ME often report heightened sensitivity to light, sound, and touch, as well as intolerance to chemicals or certain foods. These sensitivities can significantly impact daily life and contribute to social isolation.
Possible Causes of Chronic Fatigue Syndrome
The exact cause of CFS/ME is unknown, and it is likely that multiple factors contribute to its development. Research suggests a combination of genetic, environmental, and physiological factors may be involved.
- Viral Infections
Many cases of CFS/ME appear to be triggered by viral infections, such as Epstein-Barr virus (EBV), human herpesvirus 6 (HHV-6), and enteroviruses. While not everyone who contracts these infections develops CFS/ME, they may act as a trigger in genetically predisposed individuals.
- Immune System Dysfunction
Abnormalities in immune function, such as elevated levels of inflammatory markers and dysregulation of cytokines, have been observed in individuals with CFS/ME. This suggests that the immune system may play a role in the pathogenesis of the condition.
- Hormonal Imbalances
Some studies have indicated that individuals with CFS/ME may have abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body’s stress response. These hormonal imbalances could contribute to the fatigue and other symptoms experienced by those with CFS/ME.
- Genetic Factors
There is evidence to suggest that genetic predisposition plays a role in the development of CFS/ME. Twin studies have shown that CFS/ME is more common in monozygotic (identical) twins than in dizygotic (fraternal) twins, indicating a potential hereditary component.
- Psychological Factors
While CFS/ME is not a psychological disorder, psychological factors such as stress, trauma, and emotional distress can contribute to the onset and progression of the illness. However, these factors do not cause the condition but may influence its severity and course.
Diagnosis of Chronic Fatigue Syndrome
Diagnosing CFS/ME is challenging due to the lack of a definitive test and the overlap of symptoms with other conditions. The diagnosis is primarily clinical, based on the exclusion of other potential causes and the presence of specific criteria.
- Diagnostic Criteria
The most commonly used diagnostic criteria are the 1994 Centers for Disease Control and Prevention (CDC) criteria, the Canadian Consensus Criteria, and the Institute of Medicine (IOM) criteria. These criteria include the presence of unexplained fatigue lasting for more than six months, post-exertional malaise, unrefreshing sleep, and either cognitive impairment or orthostatic intolerance.
- Exclusion of Other Conditions
Before diagnosing CFS/ME, it is essential to rule out other medical and psychiatric conditions that could explain the symptoms, such as hypothyroidism, sleep apnea, depression, and autoimmune disorders.
- Comorbid Conditions
Many individuals with CFS/ME have comorbid conditions such as fibromyalgia, irritable bowel syndrome (IBS), and migraines. Identifying and managing these comorbidities is crucial for improving overall quality of life.
Challenges in Diagnosis
One of the biggest challenges in diagnosing CFS/ME is the lack of awareness and understanding among healthcare providers. Many patients experience long delays in diagnosis and may be misdiagnosed with other conditions, such as depression or anxiety. This can lead to inappropriate treatments and further deterioration of health.
Managing Symptoms of Chronic Fatigue Syndrome
Currently, there is no cure for CFS/ME, and treatment is primarily focused on symptom management and improving quality of life. An individualized and multidisciplinary approach is often necessary to address the diverse symptoms experienced by patients.
- Lifestyle Management
Pacing and Activity Management: Pacing, or the management of activity levels to avoid exacerbating symptoms, is a critical strategy for individuals with CFS/ME. This involves balancing periods of activity with rest and avoiding overexertion, which can lead to post-exertional malaise.
Sleep Hygiene: Improving sleep quality through good sleep hygiene practices, such as maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants, can help alleviate some symptoms of CFS/ME.
Diet and Nutrition: A balanced diet that supports overall health is important for individuals with CFS/ME. Some may benefit from specific dietary modifications, such as avoiding foods that trigger symptoms or cause sensitivities.
- Medications
While there are no FDA-approved medications specifically for CFS/ME, various medications can be used to manage individual symptoms:
Pain Management: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may help alleviate muscle and joint pain. For more severe pain, prescription medications such as low-dose antidepressants or anticonvulsants may be recommended.
Sleep Aids: For those with significant sleep disturbances, medications such as melatonin, low-dose tricyclic antidepressants, or non-benzodiazepine sleep aids may be helpful.
Orthostatic Intolerance: Medications that increase blood volume, such as fludrocortisone, or those that regulate heart rate and blood pressure, such as beta-blockers, may be used to manage symptoms of orthostatic intolerance.
- Cognitive Behavioral Therapy (CBT)
CBT is a psychological treatment that has been shown to help some individuals with CFS/ME manage their symptoms. It focuses on changing unhelpful thought patterns and behaviors related to illness management. However, it is not a cure and may not be suitable for all patients.
- Graded Exercise Therapy (GET)
GET involves gradually increasing physical activity levels under
the supervision of a healthcare professional. It aims to improve physical fitness and reduce deconditioning. However, GET is controversial within the CFS/ME community, as it can exacerbate symptoms in some individuals. It is essential that any exercise program be carefully tailored and monitored.
- Alternative and Complementary Therapies
Many individuals with CFS/ME explore alternative therapies, such as acupuncture, massage, and yoga, to manage their symptoms. While these approaches may provide symptom relief for some, it is essential to approach them cautiously and in conjunction with conventional medical care.
Living with Chronic Fatigue Syndrome
Living with CFS/ME can be incredibly challenging due to the unpredictable nature of the illness and the impact on daily life. Many individuals experience social isolation, difficulty maintaining employment, and a lack of understanding from family, friends, and healthcare providers.
- Coping Strategies
Support Networks: Building a support network of family, friends, and healthcare providers who understand the challenges of CFS/ME can be invaluable. Support groups, both online and in-person, provide a sense of community and shared experience.
Mindfulness and Relaxation Techniques: Practices such as mindfulness meditation, deep breathing exercises, and gentle yoga can help manage stress and improve emotional well-being.
Education and Advocacy: Educating oneself about CFS/ME and advocating for proper care and accommodations can empower individuals and improve their interactions with the healthcare system and workplace.
- Impact on Family and Relationships
CFS/ME can also take a toll on relationships with family and friends, who may struggle to understand the limitations imposed by the illness. Open communication and educating loved ones about the nature of the condition are essential for maintaining supportive relationships.
- Work and Disability
Maintaining employment can be particularly challenging for those with CFS/ME due to fluctuating symptoms and the need for frequent rest. Some individuals may need to reduce their working hours, change to less demanding roles, or apply for disability benefits if they are unable to work.
Research and Future Directions
Despite the challenges in understanding and treating CFS/ME, research is ongoing. Recent studies have focused on identifying biomarkers, understanding the role of the immune system, and developing targeted treatments. The use of technologies such as neuroimaging and genomics holds promise for unraveling the complexities of the condition.
- Biomarker Discovery
Identifying biomarkers for CFS/ME could revolutionize the diagnosis and treatment of the condition. Potential biomarkers being studied include cytokine profiles, neuroimaging findings, and metabolomic patterns.
- Treatment Development
Ongoing research into the pathophysiology of CFS/ME is paving the way for the development of targeted treatments. Trials of antiviral medications, immune-modulating therapies, and treatments aimed at improving mitochondrial function are currently underway.
- Increased Awareness and Education
Efforts to raise awareness and educate healthcare professionals about CFS/ME are essential for improving the diagnosis and care of individuals with the condition. Advocacy groups and patient organizations play a crucial role in this endeavor.
Conclusion
Chronic Fatigue Syndrome/Myalgic Encephalomyelitis is a complex and often misunderstood condition that significantly impacts the lives of those affected. While much remains to be understood about its causes and treatment, ongoing research and increased awareness offer hope for improved diagnosis and management in the future. For individuals living with CFS/ME, a comprehensive and compassionate approach that addresses both physical and emotional needs is essential for enhancing quality of life.
-
 Press Release6 days ago
Press Release6 days agoCrypto WINNAZ Launches First On-Chain Yield Engine for Meme Coins, Enabling 20x–300x Returns
-

 Press Release4 days ago
Press Release4 days agoBellarium ($BEL) Price Prediction: Could It Hit $5 by 2026?
-
 Press Release2 days ago
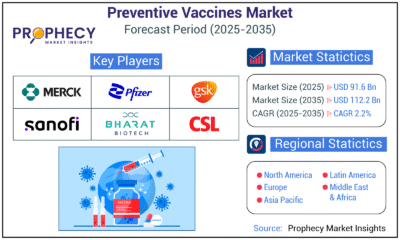
Press Release2 days agoPreventive Vaccines Market to Witness Strong Growth by 2035
-
 Press Release21 hours ago
Press Release21 hours agoClinical Trials Market Set for Robust Growth, Driven by Drug Development Surge and Digital Innovation
-

 Business3 days ago
Business3 days agoHow Managed IT Solutions Help Small Teams Compete at Enterprise Scale
-
 Press Release2 days ago
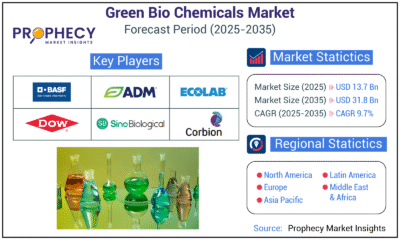
Press Release2 days agoGreen Bio Chemicals Market Poised for Sustainable Growth amidst Global Shift to Eco-Friendly Alternatives by 2035
-

 Press Release2 days ago
Press Release2 days agoFill-Finish Pharmaceutical Contract Manufacturing Market Expected to Flourish Amid Biopharmaceutical Boom and Global Outsourcing Trend by 2035
-
 Press Release2 days ago
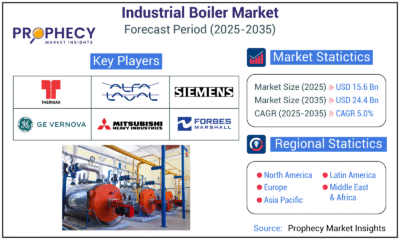
Press Release2 days agoIndustrial Boiler Market Expected to Surpass USD 24.4 Billion by 2035 Amid Growing Demand for Energy Efficiency and Industrialization