Public Health
Asthma and Allergies: Managing Symptoms and Improving Quality of Life

Asthma and allergies are two of the most prevalent chronic conditions worldwide, impacting millions of lives across all age groups. They are closely linked, with allergies often being a significant trigger for asthma symptoms. The complex interplay between these conditions can lead to significant discomfort and, if not managed properly, can substantially reduce one’s quality of life. This article provides a comprehensive exploration of asthma and allergies, their causes, symptoms, and management strategies, focusing on improving the quality of life for those affected.
Understanding Asthma
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to difficulty breathing. The condition can range from mild to severe and is often episodic, with symptoms including shortness of breath, wheezing, chest tightness, and coughing, particularly at night or early morning. The exact cause of asthma remains elusive, but it is believed to result from a combination of genetic and environmental factors.
Types of Asthma
Asthma can be categorized into several types based on triggers, severity, and underlying causes:
Allergic Asthma: This is the most common form of asthma, triggered by allergens such as pollen, pet dander, dust mites, or mold. Individuals with allergic asthma often have a history of other allergic conditions, such as allergic rhinitis or eczema.
Non-Allergic Asthma: Unlike allergic asthma, this type is not triggered by allergens. Instead, it is often brought on by factors like stress, exercise, cold air, smoke, or respiratory infections.
Exercise-Induced Asthma (EIA): Also known as exercise-induced bronchoconstriction (EIB), this type of asthma is triggered by physical exertion. It often occurs after vigorous exercise and is more common in people with other types of asthma.
Occupational Asthma: This type is directly related to the workplace environment. Exposure to dust, chemicals, fumes, or other irritants can lead to asthma symptoms in susceptible individuals.
Aspirin-Induced Asthma: Some people with asthma have a sensitivity to aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), which can trigger severe asthma symptoms.
Causes and Risk Factors
Asthma is influenced by a complex interplay of genetic predisposition and environmental triggers:
- Genetics: Asthma often runs in families, suggesting a strong genetic component. Specific genes have been associated with the risk of developing asthma, especially genes related to immune system regulation and inflammatory response.
- Environmental Factors: Exposure to allergens (such as pollen, dust mites, or pet dander), respiratory infections during childhood, air pollution, tobacco smoke, and occupational irritants can increase the risk of developing asthma.
- Obesity: There is evidence suggesting a link between obesity and asthma. The inflammatory processes involved in obesity may contribute to asthma symptoms.
- Gender and Age: Asthma is more common in boys during childhood, but more women are affected after puberty and in adulthood.
- Other Health Conditions: Conditions such as gastroesophageal reflux disease (GERD), sinusitis, and sleep apnea can exacerbate asthma symptoms.
Understanding Allergies
Allergies occur when the immune system reacts to a foreign substance such as pollen, bee venom, or pet dander that doesn’t cause a reaction in most people. The immune system produces antibodies that identify a particular allergen as harmful, even though it isn’t. Upon exposure, the immune system’s reaction can inflame the skin, sinuses, airways, or digestive system.
Types of Allergies
Symptoms include sneezing, runny nose, itchy eyes, and congestion.
1) Respiratory Allergies: These are the most common and include allergic rhinitis (hay fever) caused by pollen, dust mites, mold spores, and pet dander.
2) Food Allergies: Some people have adverse reactions to certain foods such as nuts, shellfish, milk, eggs, wheat, and soy. Symptoms can range from mild (hives, itching) to severe (anaphylaxis, a life-threatening reaction).
3) Skin Allergies: Conditions such as eczema (atopic dermatitis), contact dermatitis, and urticaria (hives) are common forms of skin allergies.
4) Insect Sting Allergies: Some individuals are allergic to stings from bees, wasps, or ants, which can lead to swelling, itching, or, in severe cases, anaphylaxis.
5) Drug Allergies: Certain medications, such as penicillin or sulfa drugs, can trigger allergic reactions in some people.
Causes and Risk Factors
Like asthma, allergies are the result of both genetic and environmental factors:
- Genetic Predisposition: If one or both parents have allergies, there is a higher likelihood that their children will have them as well.
- Environmental Exposures: Early exposure to potential allergens, particularly in the first few years of life, can increase the risk of developing allergies.
- Immune System Response: Allergies are primarily an overreaction of the immune system to harmless substances. Why this happens is not fully understood but involves both genetic and environmental components.
The Link Between Asthma and Allergies
Asthma and allergies often occur together, with allergies being a significant trigger for asthma symptoms. When an individual with allergic asthma is exposed to allergens like pollen, dust mites, or pet dander, their immune system responds by releasing substances that can cause airway inflammation and constriction, leading to asthma symptoms. The relationship between these conditions is so intertwined that about 60-80% of individuals with asthma also have allergic rhinitis.
Diagnosis and Management of Asthma and Allergies
A proper diagnosis is crucial for effective management and improving the quality of life for individuals with asthma and allergies. Diagnosis usually involves a combination of medical history, physical examination, lung function tests, and allergy testing.
Diagnostic Tools
Spirometry: This test measures the amount and speed of air a person can exhale, helping to determine lung function and the presence of obstructive airway conditions such as asthma.
Peak Flow Meter: This device helps monitor asthma control by measuring how quickly one can expel air from the lungs. Lower-than-usual readings may indicate worsening asthma.
Allergy Testing: Skin prick tests or blood tests (such as the specific IgE test) help identify specific allergens that may trigger allergic reactions or asthma symptoms.
Methacholine Challenge Test: This test is used when asthma diagnosis is unclear. Methacholine is an agent that can narrow the airways, and if this narrowing is reversible after inhaling a bronchodilator, asthma is likely present.
Management Strategies for Asthma
Effective asthma management requires a comprehensive approach that includes medication, lifestyle changes, and ongoing monitoring:
Medications:
- Quick-Relief Medications: These are bronchodilators (like albuterol) that relax the muscles around the airways, providing immediate relief from acute symptoms.
- Long-Term Control Medications: Inhaled corticosteroids (such as fluticasone), leukotriene modifiers (such as montelukast), and long-acting beta-agonists (LABAs like salmeterol) help reduce inflammation and prevent symptoms over time.
- Biologic Therapies: For severe asthma, biologics such as omalizumab, mepolizumab, or dupilumab can target specific pathways involved in the inflammatory process.
Lifestyle and Environmental Changes:
- Allergen Avoidance: Identifying and minimizing exposure to known triggers, such as dust mites, mold, pollen, or pet dander, is essential for managing symptoms.
- Smoking Cessation: Avoiding smoking and secondhand smoke is crucial, as tobacco smoke is a potent trigger for asthma exacerbations.
- Exercise and Weight Management: Regular exercise can help improve lung function and overall health, but it’s important for those with exercise-induced asthma to take preventive measures. Maintaining a healthy weight can reduce asthma severity.
Asthma Action Plan; Creating a personalized asthma action plan with healthcare providers helps individuals recognize worsening symptoms, understand medication use, and know when to seek emergency care.
Management Strategies for Allergies
The management of allergies focuses on avoiding known allergens, managing symptoms, and sometimes undergoing treatments to desensitize the body to certain triggers:
Medications:
- Antihistamines: These medications (such as cetirizine or loratadine) block histamine, a substance released during allergic reactions, thereby reducing symptoms like sneezing, itching, and runny nose.
- Decongestants: Medications like pseudoephedrine relieve nasal congestion but are usually not recommended for long-term use.
- Corticosteroids: Nasal sprays (like fluticasone) or creams can help reduce inflammation in allergic rhinitis and skin allergies, respectively.
- Epinephrine (Adrenaline): For severe allergic reactions (anaphylaxis), immediate injection of epinephrine is critical.
Allergy Shots (Immunotherapy):
This long-term treatment involves gradually increasing doses of the allergen to build tolerance in the immune system. It is especially effective for individuals with severe allergic rhinitis or insect sting allergies.
Lifestyle and Environmental Modifications:
- HEPA Filters: High-efficiency particulate air (HEPA) filters can help remove allergens from the air in homes.
- Frequent Cleaning: Regularly washing bedding, vacuuming with HEPA filters, and reducing indoor humidity can help minimize dust mites and mold growth.
Dietary Changes For food allergies, strict avoidance of allergenic foods is necessary. It is essential to read food labels carefully and understand the risk of cross-contamination.
Improving Quality of Life for Individuals with Asthma and Allergies
While asthma and allergies are chronic conditions, proper management and lifestyle adjustments can significantly improve an individual’s quality of life. Here are some key strategies:
Patient Education and Empowerment: Educating patients about their conditions, medication management, and avoidance strategies empowers them to take control of their health. Informed patients are better equipped to recognize early signs of exacerbations and understand when to seek medical help.
Adherence to Treatment Plans: Consistency in following prescribed treatment plans, including regular use of controller medications and adherence to allergen avoidance strategies, is crucial for preventing flare-ups and improving overall well-being.
Regular Follow-up with Healthcare Providers: Regular check-ups help in monitoring the progression of the disease, adjusting treatment plans as needed, and ensuring optimal control of symptoms.
Utilizing Technology: Smartphone apps and digital tools can help patients track symptoms, medication use, and peak flow readings, providing valuable information to healthcare providers for better disease management.
Support Systems and Counseling: Emotional and psychological support from family, support groups, or counselors can help individuals cope with the daily challenges of living with chronic conditions like asthma and allergies.
Access to Emergency Care: Ensuring that patients know when and how to access emergency care can prevent complications from severe asthma attacks or anaphylactic reactions.
Emerging Research and Future Directions
The field of asthma and allergy research is rapidly evolving, with several promising developments aimed at improving the quality of life for affected individuals:
Precision Medicine: Advances in genomics and personalized medicine are helping to tailor treatments based on individual genetic profiles, leading to more effective management of asthma and allergies.
Biologic Therapies: New biologics targeting specific inflammatory pathways in asthma are being developed, offering hope for those with severe, treatment-resistant asthma.
Microbiome Research: Studies are increasingly focusing on the role of the microbiome in asthma and allergies. Understanding the interplay between gut bacteria and the immune system may pave the way for innovative treatments.
Environmental Interventions: Research is exploring how modifying indoor and outdoor environments can reduce the prevalence and severity of asthma and allergies, especially in urban settings.
Telemedicine and Remote Monitoring: The rise of telemedicine and wearable devices allows for continuous monitoring of symptoms, making healthcare more accessible and personalized.
Conclusion
Asthma and allergies are intertwined chronic conditions that require a comprehensive, individualized approach to management.
With proper diagnosis, medication, lifestyle adjustments, and education, individuals with asthma and allergies can lead full, active lives. Continued research and advances in treatment offer hope for more effective therapies and improved quality of life for millions worldwide.
The journey towards optimal management is a partnership between patients, healthcare providers, and the broader community, emphasizing the importance of awareness, advocacy, and innovation.
-

 Press Release6 days ago
Press Release6 days agoNura Labs Files Revolutionary Patent: AI-Powered Wallet Solves the $180 Billion Crypto Staking Complexity Crisis
-
 Press Release4 days ago
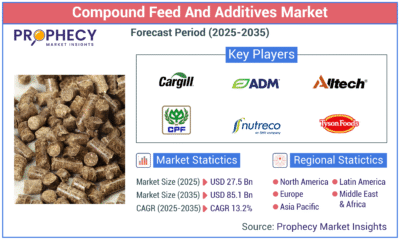
Press Release4 days agoGlobal Compound Feeds and Additives Industry Report: Market Expansion and Competitive Insights to 2035
-

 Technology4 days ago
Technology4 days agoWhat to Know Before Switching Cell Phone Network Services in 2025
-
 Press Release3 days ago
Press Release3 days agoCrypto WINNAZ Launches First On-Chain Yield Engine for Meme Coins, Enabling 20x–300x Returns
-

 Press Release7 hours ago
Press Release7 hours agoBellarium ($BEL) Price Prediction: Could It Hit $5 by 2026?
-

 Press Release6 hours ago
Press Release6 hours agoWhy Alaxio (ALX) Is a Top Pick for Smart Crypto Investors