Health & Fitness
The Link Between Depression and Anxiety

One of the most pressing concerns in mental health is the high degree of comorbidity between depression and anxiety disorders. That is to say, they often occur together in the same individual, making it complicated to tease apart their distinct characteristics and manifestations. While each disorder has its own diagnostic criteria and symptoms, their comorbidity suggests a deeper, interconnected relationship.
Many of us imagine mental health conditions existing as solitary entities, isolated within the vast spectrum of human experience. However, this perspective is challenged by the overwhelming evidence that mental health disorders often intersect and interact in complex ways that defy easy categorization. When two disorders such as depression and anxiety co-occur, this comorbidity requires us to reconsider not just the individual impact of each disorder, but also their synergistic effect on overall well-being.
The interrelatedness of depression and anxiety is not just academic—it has significant implications for treatment and long-term management. Patients grappling with both conditions frequently report a more protracted recovery period and a higher likelihood of relapse. Therefore, understanding the link between these two disorders is crucial for developing more effective treatment strategies.
Mental Health: A Dynamic Continuum
It’s crucial to recognize that mental health is not a static state but a dynamic continuum, influenced by a host of factors including genetics, environmental conditions, and lifestyle choices. For someone experiencing both depression and anxiety, this dynamic nature becomes all the more complex. One’s mental state fluctuates between depressive episodes characterized by low mood, lethargy, and lack of motivation, and periods of anxiety marked by excessive worry, fears, and physical symptoms like heart palpitations.
While depression can sap the energy and will to engage in life’s activities, anxiety can produce an excessive focus on potential threats, leading to hypervigilance and restlessness. These seemingly opposing symptoms can coalesce into a debilitating cycle where one disorder exacerbates the other, often leading to additional complications such as insomnia, substance abuse, and social withdrawal.
Panic Attacks: An Ominous Intersection
An especially troubling symptom that may arise from the comorbidity of depression and anxiety is the occurrence of panic attacks. These intense episodes of fear and dread are often accompanied by physical symptoms such as chest pain, shortness of breath, and dizziness. Panic attacks can serve as a dramatic focal point where the insidious characteristics of both depression and anxiety collide. The overwhelming despair of depression joins forces with the frenetic worry of anxiety, culminating in a volatile emotional state that is both physically and psychologically exhausting.
This convergence of symptoms not only amplifies the individual’s distress but also complicates efforts to identify a clear path toward recovery. Panic attacks often serve as a catalyst for further emotional disturbance, creating a feedback loop that intensifies both depression and anxiety.
Stress: The Common Ground
Stress serves as a common underpinning factor that can both trigger and exacerbate the symptoms of depression and anxiety. Modern life is fraught with stressors, from work pressures and interpersonal conflicts to financial insecurities and health concerns. For those predisposed to mental health conditions, chronic stress can tip the balance from occasional mood fluctuations into the realm of clinical disorders.
Stress hormones like cortisol can directly affect neurotransmitter levels in the brain, thereby influencing mood and emotional well-being. Over time, chronic stress can lay the groundwork for the onset of depression and anxiety, often in tandem, thereby increasing the complexity of both diagnosis and treatment. Stress management, therefore, becomes a cornerstone in the holistic approach to treating these comorbid conditions.
Treatment: Tailoring a Multi-Pronged Approach
Addressing the comorbidity of depression and anxiety requires a multi-pronged approach that moves beyond the conventional one-size-fits-all solutions. Effective treatment must not only aim at alleviating the individual symptoms but also consider the complex interaction between the two disorders. A combination of medication, such as antidepressants or anxiolytics, and psychotherapy is often recommended. Cognitive-behavioral therapy (CBT), in particular, has shown promise in treating both conditions by helping individuals recognize and change destructive thought patterns and behaviors.
Integrating lifestyle changes like regular exercise, a balanced diet, and adequate sleep can also be beneficial in managing the symptoms of both disorders. This comprehensive approach aims to equip individuals with the tools they need to break the debilitating cycle perpetuated by the co-occurrence of depression and anxiety, leading to a more fulfilling and balanced life.
Network Analysis of Depression and Anxiety: A Crucial Study
For those interested in a deeper understanding of the interconnectedness of depression and anxiety symptoms, the research article titled “Network analysis of depression and anxiety symptom relationships in a psychiatric sample” offers invaluable insights. Published in Psychological Medicine, this study explores the symptom-level interactions between depression and anxiety. Instead of treating these disorders as separate entities, the authors adopt a network approach to examine how individual symptoms relate to one another, thereby providing a comprehensive picture of the underlying structure of these comorbid conditions.
This research distinguishes itself by breaking away from traditional diagnostic categories to study how symptoms interact in a web-like structure. By identifying the most influential symptoms, healthcare professionals can target them for more effective interventions. This approach contrasts with other notable research efforts that typically categorize symptoms under broad diagnostic labels, thereby missing out on the interconnected nature of individual symptoms.
The network analysis methodology employed in this study stands in complement to other approaches, such as the symptom-cluster models, which consider groups of symptoms but often fail to capture the dynamic relationships between them. For instance, previous research has typically looked at depression and anxiety through the lens of their respective symptom clusters—like affective, cognitive, and somatic symptoms for depression, and physiological arousal and excessive worrying for anxiety. While these models provide a useful framework for diagnosis and treatment, they can sometimes overlook the fluid and interacting nature of symptoms, especially when the two disorders co-exist.
Therefore, the study serves as an important counterpoint, advocating for a more interconnected understanding of depression and anxiety, which can guide healthcare providers in delivering targeted and effective treatments. Given the substantial comorbidity between depression and anxiety, understanding this complex web of symptoms could be a game-changer in mental health care.
The Role of Social Support in Modulating the Anxiety-Depression Relationship
The role of social support in mental health has long been recognized, and its impact is particularly noteworthy in the context of comorbid conditions like depression and anxiety. The research paper titled “Social Support as a Moderator of the Relationship between Anxiety and Depression: An Empirical Study with Adult Survivors of Wenchuan Earthquake” takes this understanding a step further by exploring how social support can act as a moderating factor between the two disorders. According to the study, individuals with strong social support systems were found to have a less intense relationship between their anxiety and depression symptoms, compared to those with weaker social networks. This points to the buffering effect that a supportive environment can provide against the severity and interconnectedness of these mental health conditions.
This research adds another layer to our comprehension of the depression-anxiety dynamic by underscoring the protective qualities of social support. It aligns well with other studies that have shown the benefits of social engagement in improving mental health outcomes, but uniquely emphasizes how such support can specifically alter the interplay between anxiety and depression symptoms. A supportive social environment may not only ease the individual symptoms of each condition but also temper the cyclical exacerbation of symptoms when both disorders co-occur. Therefore, fostering robust social support systems could be a strategic component in a comprehensive treatment plan for individuals grappling with both depression and anxiety.
Authors: Doctor Ashok Bharucha and David Dardashti
-

 Destinations4 days ago
Destinations4 days agoSave Money in London: Insider Tips for Budget Travellers
-

 USA News3 days ago
USA News3 days agoWhat Is The Current Us Elections Rating And Who Is Leading The Polls?
-
 Technology5 days ago
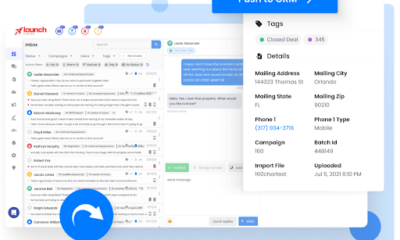
Technology5 days agoEnhancing Lead Management and Text Marketing with Launch Control’s All-in-One CRM
-

 Europe News3 days ago
Europe News3 days agoSee Rome on a Budget: History and Culture Without the Cost
-

 Travel3 days ago
Travel3 days agoHow to Make Friends in Southeast Asia Hostels: A Guide for Solo Travellers
-

 Climate Change3 days ago
Climate Change3 days agoCuba Faces Nationwide Power Grid Collapse Amidst Ongoing Crisis
-

 Travel3 days ago
Travel3 days agoSafe Travel in Mexico: Tips for a Hassle-Free Trip
-

 Destinations4 days ago
Destinations4 days agoArgentina Travel Guide: Tango, Wine, and Natural Wonders