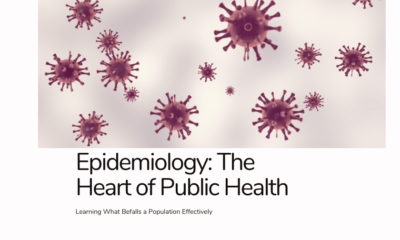
Public Safety
Infectious Disease Outbreaks: How to Protect Your Community

Infectious diseases are a persistent global threat, capable of disrupting lives, economies, and public health systems. From the COVID-19 pandemic to more localized outbreaks of diseases like Ebola and Monkeypox, the past few decades have illustrated the devastating consequences of uncontrolled outbreaks. These crises emphasize the critical need for communities to prepare for and respond effectively to infectious disease outbreaks to minimize their impact on human health and social systems.
In this report, we will explore how communities can best protect themselves from these emerging threats, delving into measures that range from individual action to policy-level responses, as well as the essential role that public health infrastructure plays in combating outbreaks.
Current Global Threats: Infectious Diseases of 2023
The world is currently grappling with multiple infectious disease outbreaks, underscoring the urgency for enhanced community protection strategies. According to the Centers for Disease Control and Prevention (CDC), some of the most notable outbreaks include the ongoing fight against COVID-19 variants, the resurgence of polio in select regions, and emerging threats from Marburg virus outbreaks in parts of Africa. In 2023, outbreaks of antibiotic-resistant bacteria and seasonal influenza continue to pose significant risks, especially in low-resource areas and communities lacking robust healthcare infrastructures.
These outbreaks are not confined to one region or continent. Infectious diseases have the potential to spread across borders in a matter of hours, making it vital to establish global cooperation to contain them at their source.
How Communities Can Protect Themselves
Strengthening Local Public Health Infrastructure
A community’s first line of defense against infectious disease outbreaks is a strong and adaptable public health infrastructure. This involves having trained healthcare professionals, well-equipped medical facilities, and the capacity to deploy rapid response measures such as testing, vaccination, and treatment. The CDC, through initiatives like the Public Health Emergency Preparedness (PHEP) program, has been instrumental in funding local governments and health organizations to build these capacities. The program supported responses to COVID-19 and continues to aid preparedness efforts for future pandemics.
Public health agencies need to enhance their capability to forecast and model outbreaks. The ForeSITE (Forecasting and Surveillance of Infectious Threats and Epidemics) initiative at the University of Utah is one example of how predictive modeling tools are being used to guide decision-making in local communities. These tools allow healthcare providers to forecast patient surges, manage vaccination distribution, and monitor when interventions such as mask mandates or lockdowns may be necessary.
Community Engagement and Education
Protecting a community starts with educating its members about preventive measures and the significance of public health guidelines. Hand hygiene, mask-wearing, and vaccination remain some of the most effective personal preventive measures. The CDC continues to stress the importance of public awareness, especially for diseases transmitted through close contact, like COVID-19 and Monkeypox.
For example, communities need to understand the value of vaccines, not just in preventing COVID-19 but also for seasonal flu, polio, and other preventable diseases. Resistance to vaccines, driven by misinformation, remains a significant challenge. Educational campaigns aimed at dispelling myths and providing accurate, science-based information are vital in ensuring high immunization rates.
Economic and Social Policy Interventions
Economic and social policies can be powerful tools in minimizing the impact of infectious disease outbreaks on communities. During the COVID-19 pandemic, many governments enacted economic relief programs, provided free testing and vaccinations, and enforced public health mandates such as social distancing and mask-wearing. These measures saved lives and alleviated the strain on healthcare systems.
However, future outbreaks may require tailored interventions. For example, densely populated cities may need stricter quarantine measures, while rural areas might focus more on distributing health services and education. Moreover, social inequalities, such as those experienced by low-income or minority groups, often exacerbate the spread and impact of disease. Therefore, outbreak response plans should incorporate policies that ensure equitable access to healthcare and support.
Strengthening Global Cooperation
Since infectious diseases do not respect borders, international cooperation is critical. Organizations like the World Health Organization (WHO) and the CDC’s global arms work tirelessly to support health systems worldwide, particularly in developing nations where disease outbreaks often originate. During the 2023 Marburg virus outbreak in Africa, global cooperation led to swift containment efforts, saving lives and preventing the virus from spreading further.
Efforts such as the CDC’s global outreach programs build “first lines of defense,” particularly in vulnerable regions, by providing technical expertise, funding, and equipment to respond to outbreaks. This is crucial, as an outbreak in one region can rapidly escalate into a global pandemic if not addressed early.
Using Technology and Data for Early Detection
Rapid detection of infectious diseases can halt their spread before they become widespread epidemics. Advancements in technology, such as genome sequencing, artificial intelligence (AI), and data-sharing platforms, allow for the early identification of new pathogens and emerging outbreaks.
The CDC’s Center for Forecasting and Outbreak Analytics (CFA) has been leading the charge in deploying real-time data to track the spread of infectious diseases. The network aims to provide local health officials with evidence-based information to implement timely interventions. This initiative, bolstered by partnerships with academic institutions and local health departments, has been instrumental in tailoring responses to the specific needs of diverse communities.
Developing Resilient Healthcare Systems
A well-resourced and resilient healthcare system is vital for preventing outbreaks from spiraling out of control. Communities should invest in healthcare infrastructure, ensure the availability of personal protective equipment (PPE), and streamline logistics for vaccine distribution and treatment during crises.
For instance, during the COVID-19 pandemic, some states in the U.S., such as Tennessee and Vermont, leveraged pre-existing flu exercise programs to rapidly scale their vaccination efforts for COVID-19, demonstrating the effectiveness of preparedness. Other regions have since adopted similar strategies, ensuring that stockpiles of medical supplies and healthcare worker training programs are updated regularly to handle future outbreaks.
The Way Forward
As infectious disease outbreaks continue to evolve, communities must remain vigilant, prepared, and adaptive. Building strong public health systems, engaging communities in prevention efforts, leveraging technology for early detection, and fostering global cooperation will be essential in protecting against future pandemics.
The experiences of the COVID-19 pandemic serve as a stark reminder that early detection, rapid response, and equitable distribution of healthcare resources are vital. With the ongoing support from governmental and global health institutions, communities can develop the resilience required to tackle future public health challenges effectively.
-

 Press Release6 days ago
Press Release6 days agoNura Labs Files Revolutionary Patent: AI-Powered Wallet Solves the $180 Billion Crypto Staking Complexity Crisis
-
 Press Release4 days ago
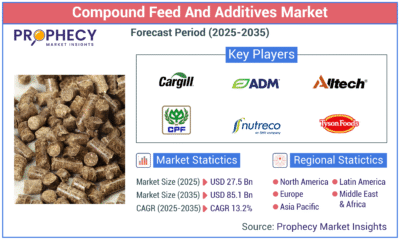
Press Release4 days agoGlobal Compound Feeds and Additives Industry Report: Market Expansion and Competitive Insights to 2035
-

 Technology4 days ago
Technology4 days agoWhat to Know Before Switching Cell Phone Network Services in 2025
-
 Press Release2 days ago
Press Release2 days agoCrypto WINNAZ Launches First On-Chain Yield Engine for Meme Coins, Enabling 20x–300x Returns