Healthcare
Dropping like Flies: The Rapid Decline of Pharmacies in the US

Far too often, we take the most convenient things in our life for granted. When you walk out of your doctor’s office, prescription in hand, you can strut to a pharmacy within a five mile radius. Now, imagine if that was taken away; if you now lived in a community where the closest pharmacy is now miles away, a far cry from the once-convenient store just around the corner. For older adults, who often juggle multiple prescriptions and rely on pharmacists for advice, this scenario is becoming increasingly common. Over the past decade, nearly 30% of pharmacies in the United States have closed their doors, and the closures are accelerating.
The result? A growing healthcare crisis where access to essential medications and vital preventative care is slipping out of reach, leaving vulnerable populations to navigate a maze of barriers that could compromise their health—and their quality of life.
The lack of access to pharmacies is presenting a major problem for millions of Americans, especially seniors. Picking up prescriptions is not just a routine errand—it’s a necessity for managing chronic illnesses such as diabetes, hypertension, and heart disease. When a pharmacy closes, it often means longer travel times and increased difficulty obtaining medications, particularly for those who no longer drive or rely on caregivers.
“The decrease in pharmacies across the US creates two distinct, but interconnected problems for Americans. Both problems lead to poorer healthcare in those communities at higher costs to everyone. The first problem communities face when they lose access to a pharmacy is they see patients struggle to properly manage conditions requiring consistent access to their medication,” asserts DoorSpace CEO Sarah M. Worthy.
While mail-order prescriptions can be a partial solution, they come with limitations. Many states impose strict regulations on mailing certain medications, especially those used to manage mental health conditions, which means patients must pick up their prescriptions in person. This can lead to dangerous interruptions in medication adherence.
“Mail delivery programs can help somewhat—but most states have regulatory restrictions in place for a number of drugs, especially drugs to manage mental health conditions, that prohibit mail delivery to patients. This means patients may skip doses for several days while they’re trying to arrange the time and transportation to get to the nearest pharmacy that may now be over an hour away, instead of 20 minutes, by car,” continue Worthy.
Missed doses can have serious consequences. For individuals managing chronic illnesses, even a short lapse in medication can lead to complications, emergency room visits, and hospitalizations. The burden then shifts to doctors and hospitals, increasing demand on an already strained healthcare system.
Beyond medication access, many pharmacies also serve as informal healthcare hubs, providing vaccinations, health screenings, and guidance on minor medical concerns. As pharmacies close, communities lose these vital services, forcing more people to seek care from overburdened primary care doctors—or worse, to forgo care altogether.
“The second problem is that many of these pharmacies are also providing some form of primary and/or preventative care, and when they close, that community loses that preventative care,” states Worthy. “These pharmacies often provide vaccinations and help advise customers on over-the-counter medications for minor ailments and injuries. Many also have an advanced nursing practitioner who comes in on a part- or full-time basis to see patients for regular primary care and non-emergency health concerns.”
As pharmacies disappear, the responsibility of filling these healthcare gaps increasingly falls on primary care physicians and hospital emergency rooms. Clinicians must spend more time addressing medication non-adherence and managing conditions that could have been controlled with proper pharmaceutical guidance. This strains an already overwhelmed healthcare workforce, leading to longer wait times and reduced quality of care.
Addressing this crisis requires both policy changes and innovative solutions. Expanding telepharmacy services, relaxing restrictions on mail-order medications, and incentivizing pharmacies to remain in underserved areas are all potential steps forward. Additionally, integrating pharmacy services into existing healthcare settings—such as within clinics and senior centers—could help bridge the gap.
-
 Press Release7 days ago
Press Release7 days agoClinical Trials Market Set for Robust Growth, Driven by Drug Development Surge and Digital Innovation
-
 Press Release7 days ago
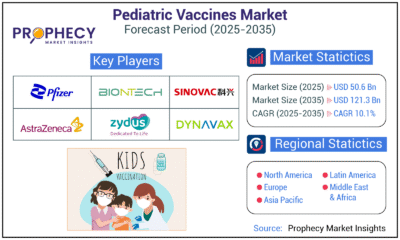
Press Release7 days agoPediatric Vaccines Market: Safeguarding Futures, Driving Growth
-

 Press Release7 days ago
Press Release7 days agoWaterproof Structural Adhesives Market: A Comprehensive Study Towards USD 10.3 Billion in 2035
-
 Press Release7 days ago
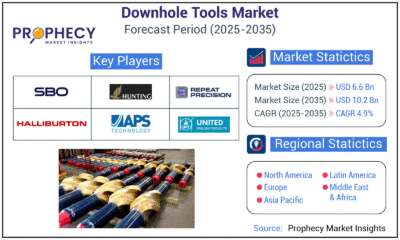
Press Release7 days agoDownhole Tools Market: Navigating Subsurface Frontiers with Precision
-
 Press Release7 days ago
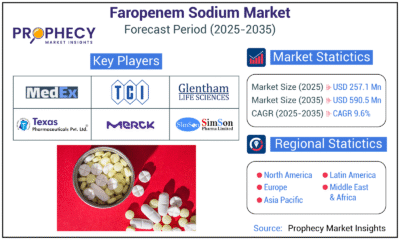
Press Release7 days agoFaropenem Sodium Market: A Potent Weapon in the Fight Against Bacterial Infections













