Public Health
Dengue Fever: Prevention and Treatment in a Changing Climate

Dengue fever, a mosquito-borne viral infection, has become a significant global health concern, particularly as climate change influences the geographical spread and intensity of its transmission. Originally confined to tropical and subtropical regions, dengue fever is now spreading to temperate zones, fueled by changing environmental conditions. The interplay between climate change and dengue epidemiology is complex, involving a myriad of factors such as temperature, precipitation, humidity, and human behavior. Let’s delve into the intricacies of dengue fever, its prevention and treatment, and how a changing climate is reshaping the global landscape of this disease.
Understanding Dengue Fever: A Primer
Dengue fever is caused by the dengue virus (DENV), which belongs to the Flaviviridae family and has four distinct serotypes: DENV-1, DENV-2, DENV-3, and DENV-4. Infection with one serotype provides lifelong immunity against that serotype but not against the others, leading to the possibility of multiple infections throughout a person’s life. Subsequent infections increase the risk of severe dengue, also known as dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS), which can be fatal if not treated promptly.
Transmission Dynamics
The primary vectors of dengue are the Aedes aegypti and Aedes albopictus mosquitoes, which thrive in urban environments and are highly adapted to human habitats. These mosquitoes are day-biting and breed in stagnant water, often found in artificial containers such as flowerpots, discarded tires, and water storage containers. The transmission cycle begins when a female mosquito bites an infected individual, ingests the virus, and then, after an incubation period of 8-12 days, becomes capable of transmitting the virus to another person through its bite.
Symptoms and Diagnosis
Dengue fever typically presents with a sudden onset of high fever, severe headache, pain behind the eyes, muscle and joint pain, nausea, vomiting, swollen glands, and a characteristic rash. These symptoms usually last for 2-7 days. Severe dengue, which can occur when the disease progresses, is marked by symptoms such as severe abdominal pain, persistent vomiting, rapid breathing, bleeding gums, fatigue, restlessness, and blood in vomit or stool.
Diagnosis of dengue is challenging due to its nonspecific symptoms, which can be mistaken for other febrile illnesses. Laboratory tests such as reverse transcriptase-polymerase chain reaction (RT-PCR), enzyme-linked immunosorbent assay (ELISA), and rapid diagnostic tests (RDTs) are used to confirm the presence of the virus or antibodies against it.
Impact of Climate Change on Dengue Fever
Climate change is a critical factor influencing the spread of dengue fever. Rising global temperatures, altered precipitation patterns, and increased frequency of extreme weather events are creating favorable conditions for mosquito breeding and virus transmission.
Temperature and Vector Proliferation
Temperature plays a crucial role in the life cycle and distribution of the Aedes mosquitoes. Warmer temperatures accelerate the development of mosquito larvae into adults, shorten the extrinsic incubation period (the time taken for the virus to become transmissible after the mosquito ingests it), and increase the frequency of mosquito feeding. Studies have shown that even a slight increase in temperature can significantly enhance vector competence and virus transmission, thus expanding the geographical range of dengue into previously unaffected areas, including higher altitudes and latitudes.
Rainfall and Breeding Habitats
Rainfall patterns also significantly impact mosquito breeding. While heavy rainfall can create new breeding sites, it can also flush out existing ones, reducing mosquito populations temporarily. Conversely, periods of drought may lead people to store water in containers, inadvertently providing breeding grounds for Aedes mosquitoes. The interplay between rainfall and temperature creates a dynamic environment that can either amplify or suppress dengue outbreaks.
Urbanization and Human Behavior
Rapid urbanization, particularly in developing countries, often leads to inadequate housing, poor waste management, and insufficient water storage facilities, all of which contribute to an increase in mosquito breeding sites. Human behavior, such as storing water in uncovered containers, and social factors like population density, also play a role in the transmission dynamics of dengue fever.
Prevention Strategies in a Changing Climate
Preventing dengue fever requires a multi-pronged approach, incorporating vector control, community engagement, and public health interventions. As climate change alters the epidemiology of dengue, adaptive strategies are essential to mitigate its impact.
Vector Control Measures
1. Source Reduction: Eliminating mosquito breeding sites is one of the most effective methods of dengue prevention. This involves removing or treating standing water in and around homes, schools, and workplaces. Regular inspection and cleaning of potential breeding sites, such as gutters, water storage containers, and flower pots, are crucial.
2. Chemical Control: The use of insecticides, such as larvicides and adulticides, is a common method of controlling mosquito populations. However, the over-reliance on chemical control can lead to the development of insecticide resistance in mosquito populations, making this approach less effective over time. Integrated vector management (IVM), which combines chemical and non-chemical methods, is recommended to sustain efficacy.
3. Biological Control: Introducing natural predators, such as fish that feed on mosquito larvae, or the use of bacteria like Wolbachia, which can reduce the ability of mosquitoes to transmit dengue, are emerging biological control strategies. Wolbachia-infected mosquitoes have shown promise in reducing dengue transmission in field trials.
4. Personal Protection: Using personal protective measures such as wearing long-sleeved clothing, applying insect repellent, and using mosquito nets, especially during peak biting times, can reduce the risk of mosquito bites.
5. Community Engagement: Community participation is vital for the success of dengue prevention programs. Educating communities about the importance of eliminating breeding sites and engaging them in vector control activities can lead to sustainable reductions in mosquito populations.
Surveillance and Early Warning Systems
Enhanced surveillance systems that monitor mosquito populations, climate conditions, and dengue cases can provide early warnings of potential outbreaks. Geographic Information Systems (GIS) and remote sensing technologies are being used to predict dengue hotspots based on environmental factors, enabling targeted interventions. Climate-based models that incorporate temperature, rainfall, and humidity data are also being developed to forecast dengue transmission risks more accurately.
Vaccination Efforts
The development of a safe and effective dengue vaccine has been a significant challenge due to the complexity of the virus and the need for protection against all four serotypes. Dengvaxia, the first dengue vaccine licensed, has shown varying efficacy and is recommended only in individuals who have previously been infected with dengue, as it can increase the risk of severe dengue in those who have not been previously exposed. Research into next-generation vaccines continues, with the goal of developing a more universally effective solution.
Treatment Options for Dengue Fever
Currently, there is no specific antiviral treatment for dengue fever. Management focuses on supportive care to alleviate symptoms and prevent complications.
Supportive Care
1. Hydration: Maintaining adequate fluid intake is crucial, especially in cases of severe dengue, where plasma leakage can lead to dehydration and shock. Oral rehydration solutions or intravenous fluids may be administered depending on the severity of the illness.
2. Pain and Fever Management: Acetaminophen (paracetamol) is recommended for managing fever and pain. Non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen should be avoided, as they can increase the risk of bleeding.
3. Monitoring for Complications: Close monitoring of patients, especially during the critical phase (when fever subsides), is essential to detect signs of severe dengue, such as bleeding, organ impairment, or shock. Early intervention can significantly reduce the risk of mortality.
Emerging Treatments and Research
Research into antiviral agents that can target the dengue virus is ongoing. Several compounds, including repurposed drugs and novel molecules, are being investigated for their potential to inhibit viral replication. Additionally, advancements in immunotherapy and host-targeted therapies may offer new avenues for the treatment of dengue in the future.
Challenges in the Fight Against Dengue
The fight against dengue fever is fraught with challenges, many of which are exacerbated by climate change and socioeconomic factors.
Insecticide Resistance
The widespread use of insecticides has led to the emergence of resistant mosquito populations in many regions. Resistance reduces the efficacy of vector control programs and necessitates the development of new insecticides or alternative control strategies.
Vaccine Hesitancy and Access
The rollout of Dengvaxia was marred by controversy due to safety concerns, leading to vaccine hesitancy and reduced public trust in dengue vaccination programs. Ensuring equitable access to future vaccines and addressing public concerns through transparent communication will be critical for the success of vaccination efforts.
Health System Capacity
Many countries affected by dengue have limited healthcare resources, making it difficult to manage large outbreaks. Strengthening health systems, improving diagnostic capabilities, and training healthcare workers are essential to effectively respond to dengue epidemics.
Climate Change Adaptation
Adapting to the changing dynamics of dengue transmission requires a coordinated effort across sectors, including health, environment, and urban planning. Developing climate-resilient health systems and incorporating climate considerations into public health policies are necessary steps to mitigate the impact of climate change on dengue transmission.
Conclusion
Dengue fever, once confined to specific tropical regions, is now a global health threat, with its reach and intensity being shaped by the changing climate. Prevention and treatment strategies must evolve in response to these changes, integrating innovative approaches and fostering international collaboration. As the world grapples with the broader impacts of climate change, addressing the complexities of dengue transmission will be crucial to safeguarding public health and preventing future outbreaks.
By investing in research, strengthening health systems, and promoting community engagement, we can build resilience against dengue fever and other climate-sensitive diseases. The road ahead is challenging, but with a comprehensive and adaptive approach, it is possible to mitigate the threat of dengue and protect vulnerable populations in a warming world.
-

 Press Release5 days ago
Press Release5 days agoBellarium ($BEL) Price Prediction: Could It Hit $5 by 2026?
-
 Press Release2 days ago
Press Release2 days agoClinical Trials Market Set for Robust Growth, Driven by Drug Development Surge and Digital Innovation
-
 Press Release3 days ago
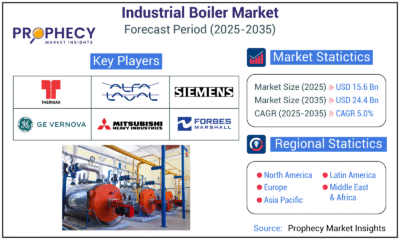
Press Release3 days agoIndustrial Boiler Market Expected to Surpass USD 24.4 Billion by 2035 Amid Growing Demand for Energy Efficiency and Industrialization
-
 Press Release3 days ago
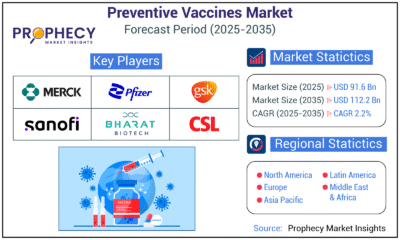
Press Release3 days agoPreventive Vaccines Market to Witness Strong Growth by 2035
-

 Business4 days ago
Business4 days agoHow Managed IT Solutions Help Small Teams Compete at Enterprise Scale
-

 Press Release3 days ago
Press Release3 days agoFill-Finish Pharmaceutical Contract Manufacturing Market Expected to Flourish Amid Biopharmaceutical Boom and Global Outsourcing Trend by 2035
-
 Press Release3 days ago
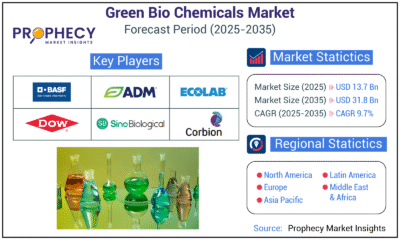
Press Release3 days agoGreen Bio Chemicals Market Poised for Sustainable Growth amidst Global Shift to Eco-Friendly Alternatives by 2035
-

 Press Release3 days ago
Press Release3 days agoPet Food Nutraceutical Market Set for Robust Expansion Amid Rising Demand for Pet Wellness by 2035