Public Health
Chronic Kidney Disease: A Comprehensive Documentary on Prevention and Management

Introduction to Chronic Kidney Disease (CKD)
Chronic Kidney Disease (CKD) is a long-term, progressive condition where the kidneys lose their ability to function effectively over time. The kidneys, two bean-shaped organs located on either side of the spine, are responsible for filtering waste, excess fluids, and toxins from the blood, producing urine, balancing electrolytes, regulating blood pressure, and contributing to red blood cell production. When these organs lose their efficiency, a dangerous buildup of wastes and fluids occurs, leading to potentially life-threatening complications.
CKD is often called a “silent killer” because it can progress without noticeable symptoms until significant kidney damage has occurred. By the time many patients receive a diagnosis, their kidney function may be severely compromised. Globally, CKD is recognized as a major public health issue, affecting an estimated 10% of the world’s population. With increasing rates of diabetes, hypertension, and obesity, three of the main risk factors for CKD, the burden of the disease is growing rapidly.
This article provides a thorough exploration of CKD, focusing on its causes, symptoms, stages, prevention strategies, and the comprehensive management required to mitigate its progression and improve patient outcomes.
Anatomy and Function of the Kidneys
Before delving into CKD, it’s important to understand the structure and function of the kidneys. Each kidney contains around a million filtering units known as nephrons, which are essential for removing waste products from the blood. A nephron consists of a filtering component called the glomerulus and a tubule that carries filtered waste to the ureters, which then lead to the bladder.
Key functions of the kidneys include:
- Waste Removal: Filtering blood to remove toxins and excess fluids, which are excreted as urine.
- Electrolyte Balance: Regulating essential minerals like sodium, potassium, and calcium, which are vital for nerve function and muscle contraction.
- Blood Pressure Regulation: Producing the hormone renin, which plays a critical role in controlling blood pressure by regulating fluid balance.
- Red Blood Cell Production: The kidneys release erythropoietin, a hormone that stimulates the production of red blood cells in response to low oxygen levels.
- Acid-Base Balance: Maintaining the body’s pH balance by removing excess acid or bases from the blood.
In CKD, these critical processes become impaired, leading to a cascade of health issues.
Causes of Chronic Kidney Disease
The most common causes of CKD include:
Diabetes: Diabetic nephropathy is one of the leading causes of CKD. High blood sugar levels can damage the tiny blood vessels in the kidneys, reducing their ability to filter waste efficiently. Over time, this damage can lead to kidney failure if left unmanaged.
Hypertension (High Blood Pressure): Hypertension damages the blood vessels in the kidneys, making it harder for them to remove waste from the blood. This, in turn, can lead to further elevation in blood pressure, creating a vicious cycle of kidney damage.
Glomerulonephritis: This is a group of diseases that cause inflammation of the glomeruli, the tiny filtering units within the kidneys. This inflammation can severely impair kidney function over time.
Polycystic Kidney Disease (PKD): An inherited disorder that causes numerous cysts to grow in the kidneys, leading to kidney enlargement and reduced function.
Obstructive Kidney Disorders: Conditions such as kidney stones, tumors, or an enlarged prostate can block the flow of urine, causing back pressure that damages the kidneys.
Autoimmune Diseases: Conditions like lupus and vasculitis can cause the body’s immune system to attack kidney tissues, leading to inflammation and scarring.
Infections: Repeated kidney infections, or pyelonephritis, can damage kidney tissues and impair kidney function over time.
Toxins and Medications: Long-term exposure to certain drugs, including nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics, as well as toxins such as heavy metals, can lead to chronic kidney damage.
Stages of Chronic Kidney Disease
CKD is classified into five stages based on the Glomerular Filtration Rate (GFR), a measure of how well the kidneys are filtering blood. The GFR is calculated based on factors such as age, gender, race, and serum creatinine levels (a waste product filtered by the kidneys).
Stage 1 (Normal or High GFR: ≥90 mL/min): At this stage, there is kidney damage with normal kidney function. Patients may have mild signs of kidney damage, such as protein in the urine, but the overall function of the kidneys remains intact. Early detection at this stage is crucial for preventing further damage.
Stage 2 (Mild CKD, GFR: 60-89 mL/min): There is a slight reduction in kidney function, but symptoms may still be mild or absent. Patients may begin to show more protein in the urine or develop hypertension. Lifestyle modifications and medication can help slow disease progression at this stage.
Stage 3 (Moderate CKD, GFR: 30-59 mL/min): Kidney function is moderately reduced, and symptoms like fatigue, swelling (edema), and changes in urine output may become more apparent. Management at this stage focuses on controlling blood pressure, blood sugar, and other risk factors to slow the progression to more severe stages.
Stage 4 (Severe CKD, GFR: 15-29 mL/min): At this stage, kidney function is severely reduced, and patients may begin to experience complications such as anemia, bone disease, and cardiovascular issues. Preparations for dialysis or a kidney transplant often begin at this stage, as the kidneys are nearing complete failure.
Stage 5 (End-Stage Renal Disease, GFR: <15 mL/min): The kidneys have lost nearly all of their filtering capacity, and patients require dialysis or a kidney transplant to survive. Symptoms are severe, and without treatment, this stage is life-threatening.
Symptoms of Chronic Kidney Disease
CKD often progresses silently, with symptoms becoming more apparent only in the later stages. However, as the disease advances, patients may experience the following symptoms:
- Fatigue: As the kidneys fail to remove toxins and waste, the body becomes more fatigued. Anemia, common in CKD, also contributes to extreme tiredness.
- Swelling (Edema): The kidneys regulate fluid balance, and when they are not functioning properly, excess fluid builds up in the body, causing swelling in the legs, ankles, and face.
- Changes in Urination: Patients may notice increased or decreased urine output, dark-colored urine, or blood in the urine.
- Nausea and Vomiting: The buildup of waste products in the bloodstream can lead to nausea, vomiting, and a general feeling of being unwell.
- Itchy Skin: The accumulation of waste in the blood can cause dry, itchy skin.
- Shortness of Breath: Fluid buildup in the lungs due to kidney dysfunction can lead to difficulty breathing.
- Muscle Cramps: Electrolyte imbalances, particularly low calcium and high phosphorus, can cause painful muscle cramps.
- Loss of Appetite and Weight Loss: The presence of toxins in the body can lead to a decreased appetite and unintentional weight loss.
Prevention of Chronic Kidney Disease
CKD prevention focuses on managing the underlying risk factors that contribute to kidney damage. Many cases of CKD are preventable through lifestyle modifications, regular medical checkups, and early intervention. Key prevention strategies include:
Controlling Blood Pressure
Hypertension is one of the leading causes of CKD. Maintaining optimal blood pressure levels through diet, exercise, and medication is essential for kidney health. The American Heart Association recommends keeping blood pressure below 130/80 mmHg to reduce the risk of kidney damage.
Managing Diabetes
For individuals with diabetes, controlling blood sugar levels is critical to preventing diabetic nephropathy, a leading cause of CKD. Regular monitoring of blood glucose levels, adhering to a healthy diet, and taking prescribed medications help prevent kidney damage.
Maintaining a Healthy Weight
Obesity increases the risk of both diabetes and hypertension, which can lead to CKD. Weight management through a balanced diet and regular exercise can lower the risk of CKD development.
Eating a Kidney-Friendly Diet
A healthy diet can significantly reduce the burden on the kidneys. Key dietary strategies include:
- Limiting Sodium: Reducing salt intake helps control blood pressure and prevent fluid retention, which can strain the kidneys.
- Controlling Protein Intake: High-protein diets can place extra stress on the kidneys. Limiting protein, particularly from animal sources, can reduce the risk of CKD progression.
- Limiting Processed Foods: Processed foods often contain high levels of sodium, phosphorus, and unhealthy fats, which can worsen kidney function.
Staying Hydrated
Drinking adequate water helps the kidneys filter toxins and waste products efficiently. However, overhydration should be avoided in people with advanced CKD, as it can exacerbate fluid retention.
Avoiding Overuse of Medications
Certain over-the-counter medications, such as NSAIDs (ibuprofen, aspirin), can cause kidney damage if used in excess. Limiting the use of these medications or seeking alternatives is important for kidney health.
Regular Screening and Checkups
Individuals at risk for CKD, including those with diabetes, hypertension, or a family history of kidney disease, should undergo regular kidney function tests. Early detection allows for prompt intervention to prevent further damage.
Management of Chronic Kidney Disease
Once CKD has been diagnosed, the focus shifts to slowing the progression of the disease and managing symptoms. CKD management is multi-faceted, often requiring lifestyle changes, medications, and in advanced stages, dialysis or transplantation.
1. Medications
Medications play a critical role in managing CKD and its complications:
Blood Pressure Medications: ACE inhibitors and ARBs are commonly prescribed to control blood pressure and reduce proteinuria (protein in the urine), which can slow CKD progression.
- Diabetes Medications: Tight control of blood sugar levels is crucial for people with diabetes and CKD. Newer diabetes drugs, such as SGLT2 inhibitors, have shown promise in protecting kidney function.
- Phosphate Binders: In advanced CKD, phosphate binders may be prescribed to reduce the levels of phosphorus in the blood and prevent bone disease.
- Erythropoiesis-Stimulating Agents (ESAs): To combat anemia, ESAs may be used to stimulate red blood cell production.
2. Dietary Management
Dietary modifications are essential for managing CKD:
- Low-Sodium Diet: Reducing salt intake helps manage blood pressure and prevent fluid retention.
- Controlled Protein Intake: Limiting protein consumption can reduce the workload on the kidneys.
- Potassium and Phosphorus Management: In later stages of CKD, patients may need to limit their intake of potassium and phosphorus to prevent dangerous imbalances.
- Fluid Restriction: In advanced CKD, fluid intake may need to be restricted to avoid edema and hypertension.
3. Dialysis
Dialysis is required when the kidneys are no longer able to filter waste and toxins effectively. There are two main types of dialysis:
- Hemodialysis: Blood is filtered through a machine that removes waste products and excess fluids before returning it to the body. Hemodialysis is typically performed several times a week at a dialysis center or at home with specialized equipment.
- Peritoneal Dialysis: A catheter is placed in the abdomen, and a dialysis solution is introduced into the peritoneal cavity, where it absorbs waste and toxins. The solution is then drained and replaced. Peritoneal dialysis can be performed at home.
4. Kidney Transplantation
For patients with end-stage renal disease (ESRD), kidney transplantation is often the best long-term solution. A healthy kidney from a donor is surgically implanted to take over the function of the failed kidneys. Transplant patients must take immunosuppressive medications for life to prevent organ rejection.
Psychosocial Support and CKD
The diagnosis of CKD can be emotionally challenging for patients and their families. The chronic nature of the disease, the potential for dialysis or transplantation, and the lifestyle changes required can lead to stress, anxiety, and depression. Psychosocial support, including counseling, support groups, and patient education, plays a crucial role in helping patients cope with the emotional and psychological impact of CKD.
The Global Burden of CKD
CKD is a major public health issue worldwide, affecting an estimated 850 million people. The rising prevalence of diabetes, hypertension, and obesity particularly in low- and middle-income countries is contributing to the global increase in CKD cases. In many regions, access to dialysis and transplantation is limited, and early detection and prevention efforts are inadequate.
The economic burden of CKD is also significant. The cost of dialysis and transplantation, along with the management of complications, places a heavy financial burden on healthcare systems and patients. Governments, healthcare providers, and global health organizations must prioritize CKD prevention and management to address this growing crisis.
Conclusion
Chronic Kidney Disease is a serious, progressive condition that affects millions of people worldwide. While the disease can have devastating consequences, early detection and effective management can slow its progression and improve quality of life. Prevention strategies, such as controlling blood pressure, managing diabetes, and adopting a kidney-friendly lifestyle, are critical in reducing the risk of CKD.
For individuals with CKD, a comprehensive approach to management including medications, dietary changes, and in some cases, dialysis or transplantation is essential to maintaining kidney function and overall health. With continued advancements in research, treatment, and public health initiatives, there is hope for reducing the global burden of CKD and improving outcomes for those affected by this silent but deadly disease.
-

 Press Release6 days ago
Press Release6 days agoNura Labs Files Revolutionary Patent: AI-Powered Wallet Solves the $180 Billion Crypto Staking Complexity Crisis
-
 Press Release4 days ago
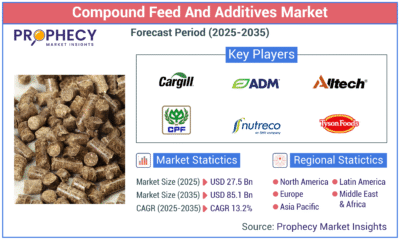
Press Release4 days agoGlobal Compound Feeds and Additives Industry Report: Market Expansion and Competitive Insights to 2035
-

 Technology4 days ago
Technology4 days agoWhat to Know Before Switching Cell Phone Network Services in 2025
-
 Press Release2 days ago
Press Release2 days agoCrypto WINNAZ Launches First On-Chain Yield Engine for Meme Coins, Enabling 20x–300x Returns